The official version of this document can be found via the PDF button.
The below content has been automatically generated from the original PDF and some formatting may have been lost, therefore it should not be relied upon to extract citations or propose amendments.
WQ.137/2019
APPROVED
WRITTEN QUESTION TO THE MINISTER FOR HEALTH AND SOCIAL SERVICES BY DEPUTY K.G. PAMPLIN OF ST. SAVIOUR
ANSWER TO BE TABLED ON TUESDAY 12th MARCH 2019
Question
Following the publication by the States in 2015 of Prevention of Suicide in Jersey: A Framework for Action 2015-2020, can the Minister confirm which actions have been implemented in relation to effective identification and planning of priorities to take forward around suicide prevention; and provide the evidence of each annual evaluation of the framework since 2015, with specific outcomes arising from the action plan, including details of the annual Prevention of Suicide Forum to communicate the progress of the framework to key stakeholders?
Answer
Progress of actions against priorities from the Prevention of Suicide in Jersey: A Framework for Action 2015-2020 has been provided in existing reports to the Health and Social Security Scrutiny Panel in 2018 in support of the review of Mental Health Services in Jersey. This is the latest information available on progress of actions:
Objective 1 |
| Action requirements | Supporting Evidence |
Improve mental health and wellbeing in vulnerable groups | 1.1 | Ensure relevant Mental Health Strategy actions take account of those groups identified as being at higher risk of suicide | Work carried out to support improved information on gov.je on emotional health and seeking help in crises for parents of young people. A wider review of how young people are influenced by social media and appropriate responses is required as part of a refresh of the suicide prevention work under the mental health implementation board. Mental Health Services carry out individual assessment of risk for self-harm and suicide with appropriate and person- specific safety planning triggered where relevant. Staff training has supported awareness and increased competence in both risk assessment and safety planning around self- harm. Services continue to have a heightened awareness of the potential increased risk of suicide amongst clients, particularly men, with addiction. Generic training regarding promoting positive mental health and resilience continues to be offered to any professional working with children and young people, thereby adding to the island offering and increasing accessibility to training given the lack of financial charge attached. Developing baseline data on awareness and stigma of mental health through Jersey Opinion and Lifestyle Survey will help support monitoring of improvements to knowledge, acceptability and access to local services supporting risk reduction. |
| 1.2 | Review and identify best model for Tier 2 early intervention in schools and colleges | The Psychology and Well-being Service (PAWBS) manages the Well-being Team, offering intervention to primary-aged children and young people for early signs of mental health and well-being challenges e.g. self-esteem, social skills, anxiety, loss. The Service also manages The Primary Mental Health Team, in operation since 2017, which promotes the necessary skill set associated with being a tier one/two mental health practitioner. A range of support is in place including: professional weekly consultation line available to support those working with children and young people; face to face consultations for families via Parentscope meetings, parent/carer workshops delivered via schools and summer workshops at the library; comprehensive training offer to any professional working with children/young people, one to one case work, liaison with CAMHS. All teams within PAWBS offer a weekly consultation line to offer advice, signposting, clinical supervision and to raise awareness, with lines operated by the Educational Psychology and Well-being Teams now available to families and young people. Mental health network meetings continue to bring charity/voluntary organisations together to share information, raise awareness, link initiatives and avoid duplication. These are chaired by the Educational Psychology Team which is also part of PAWBS. Recent introduction of the multi-agency Right Time Right Help panel with a key priority of supporting vulnerable families with early help in step down from Children's Services or following referrals from MASH. |
| 1.3 | Review existing curriculum practice and approach to mental health prevention as part of curriculum delivery in schools and colleges | Individual schools developing range of bespoke plans in meeting the needs of their own school communities and engaging with local charity Mind Jersey. Training offer available from PAWBS introducing central courses, whole staff delivery at school or bespoke packages tailored to suit needs of schools e.g. understanding and managing ADHD, supporting anxiety in children and young people. Service delivery from the Primary Mental Health Team also includes working with school staff to deliver small support groups and one to one case work alongside staff as a means of upskilling. Approximately 70 ELSAs (Emotional Literacy Support Assistants) now working in our schools. The Psychology and Well-being Service delivers a 6-day training programme and provides a continuous clinical supervision and CPD offer to support ELSAs in applying support in schools (they must attend 6 sessions per annum to remain a registered ELSA). A new training cohort offered for June and July 2019 and new additions to the training module in outdoor learning and attachment theory being devised. |
|
|
| FRIENDS training – this is a cognitive behaviour therapy- based programme designed to support early signs of anxiety/depression and is managed by PAWBS. All existing ELSAs are now trained in FRIENDS and a training offer continues to be made available with the current service offer being disseminated to other agencies. |
| 1.4 | Develop formal networks across state and 3rd Sector services to identify and maximise opportunities to coordinate approach and support | Suicide prevention steering group is a vehicle for partnership and multi-agency working. Multi-agency workshops led to the development and support of key approaches on real time suicide audit and peer support for bereavement of suicide. |
Objective 2 |
|
|
|
Reduce stigma about suicidal feelings | 2.1 | Promote sensitive reporting of suicide and portrayal of suicide in the media | Ongoing Media opportunities to raise awareness include: Annual awareness in media releases and local interest stories around National Suicide Prevention Day. Using social media at relevant potential stress points in the year to signpost to information and support for children and young people. Responding to relevant Scrutiny, Safeguarding Partnership Board and Freedom of Information enquiries. Officers liaising with editorial teams proactively ahead of inquests including the provision of good practice media guidance in suicide reporting and reactively to reporting which contravenes best practice. |
| 2.2 | Encourage seeking urgent help early to avoid emerging crisis, and promote ways of publicising help available | Business cases prepared to establish Listening Lounge; Crisis Team and Place of Safety scheduled for implementation during 2019. |
| 2.3 | Develop Information provision about suicide that helps support reduction of suicidal ideation | Will be linked to work aligned to development of 24/7 services via Listening Lounge and Crisis Service. Development of Peer Support through Mind Jersey to reduce risk amongst those people who have been bereaved by suicide. |
| 2.4 | Deliver and review effectiveness of integrated multiagency training on managing self harm and suicidal ideation, and on performing risk assessment | Development and delivery of licensed Connecting with People training programme. Up to the end of 2018, a total of 337 people from a range of agencies have been supporting people at risk of suicide. Evaluations demonstrate 96% feel more able to talk to someone in emotional distress; 91% felt more able to co-create a safety plan. Over 2018, 4 trainers have been re-accredited and 7 new trainers have been licensed to deliver training. |
Objective 3 |
|
|
|
Reduce the risk of suicide in high risk individuals | 3.1 | Identify appropriate risk assessment tools to identify high risk individuals taking into account the different drivers and risk factors for different population/age groups | Training in validated peer-assessed risk assessment approaches and tools as part of Connecting with People training programme. Priority actions to support vulnerable at risk groups has helped engage support for and the development of crisis response approaches to reduce suicide risk. Programmes currently under development include: place of safety; 24/7 crisis response; listening lounge |
| 3.2 | Developing a framework for multiagency working with those identified as high risk | Suicide prevention steering group membership and quarterly meeting supports partnership approaches and collaboration in best practice working in supporting suicide risk reduction. Review of zero suicide methodology and the latest international evidence of zero suicide methodology used to inform the provision of a position statement on considering the approach in the Jersey context and the need to apply best international evidence. |
| 3.3 | Delivering and reviewing effectiveness of integrated multiagency training for those working with high risk individuals | Completed review of prevention of suicide training and implementation of Connecting With People, awareness, risk reduction and safety planning Training Programme. Over Q4 2018, HCS has supported a full-time position to lead on the development of Prevention of Suicide priorities and lead the coordination of training. Review of training priorities and revised target groups completed for 2019 and 234 training places planned over 2019. |
| 3.4 | Monitor completed suicides annually to identify trends that will inform future interventions | Ongoing review and publication of annual suicide rates completed as per international best practice approaches. Comparisons made to other jurisdictions with relevant caveats. (* see Suicide Rates in Jersey below) Development of real time suicide audit process which monitors deaths suspected to be by suicide for any trends which could indicate related clusters and/or specific learning. The process also ensures the triggering of relevant support to family and friends. (Since commencement in 2018, the process has triggered one multi-agency meeting to review a small number of deaths suspected to be by suicide.) Serious Incident Review Panel in place through HCS overseen by Medical Director as lead for Quality & Safety. |
| 3.5 | Support the development of a multi-agency Vulnerable Adult Risk Management process | Development & Implementation of the Safeguarding Vulnerable Adults policy |
Objective 4: Improve information | 4.1 | Have in place effective local responses | Established governance arrangements in place which include policy and procedure to be followed in the event of a suicide; incident review; linked to safeguarding practice. |
and support to those bereaved or affected by suicide |
| following death by suicide & establish Safeguarding Partnership Board multiagency policy and procedure | Police Coroner's Office currently leads on triggering process of support following a suspected death by suicide, ensuring family and friends access the support available locally. |
| 4.2 | Provide information and support for families friends and colleagues who may be concerned about someone who may be at risk of suicide | Provision of information on gov.je for families on mental health/suicide risk and service support accompanied by media coverage and targeted communications through schools. Production of Help is at Hand' a bereavement by suicide resource produced in partnership with people who have lived experience of bereavement by suicide. Future development of Listening Lounge will also provide support. |
| 4.3 | Seek to secure service user feedback | Completed review of lived experience of bereavement by suicide to inform planning which involved a facilitated session and a summary report supported by follow up on findings with people with lived experience, drawing on the experiences of bereavement by suicide and opinion on support and potential gaps and areas for improvement. |
| 4.4 | Provide effective and timely support to families bereaved or affected by suicide | The co-production work with people with lived experience of bereavement in suicide culminated in the development of preferred priorities for peer support. Mind Jersey has since been engaged in a 14-month contract to pilot a peer support programme providing practical support for people who have lost a relative, loved one or close friend to suspected suicide. |
Annual reporting of progress against priorities
2015 – 2017 Reported through the Children's and Vulnerable Adults Ministerial Group. Reporting
on progress and evaluation through this route was completed in January 2017.
2016 Review of outputs presented at the multi-agency forum. Presentations were followed by
group work reviewing the initial strategic period, alongside brainstorming sessions on reform of priorities for the coming period. Forum outcomes were used in planning additional follow on multi-agency Outcomes-Based Accountability (OBA) workshops. Specific priority actions for bereavement support and services as well as priorities for vulnerable groups were identified using this OBA methodology.
2017 – 2018 Reporting on progress included and incorporated as part of the Mental Health Strategy
Steering Group with additional updates also provided to the Safeguarding Partnership Board. Annual evaluations of the Connecting with People programme have been produced and reported to the Mental Health Strategy Implementation group.
2018 – 2019 Prevention of Suicide Steering group reports on progress submitted to the Mental Health
Improvement Board. The role, remit and related terms of reference for the steering group are now under review in the context of ensuring alignment with the work of the recently convened Mental Health Improvement Board.
*Suicide Rates in Jersey
Jersey currently has a suicide rate that is comparable with other jurisdictions. The challenge in a small community such as ours is that our actual small number of deaths by suicide can fluctuate year to year and this therefore reduces the confidence in data that is seen in larger populations.
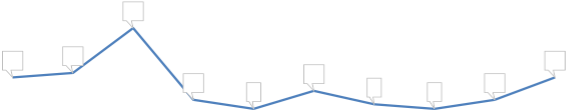
Because actual year on year numbers are subject to this variation, the annual rate is prepared using an age standardised calculation with a three-year rolling average. This allows comparison with other jurisdictions as the data accounts for any demographic differences across populations as well as allowing a clearer picture of any trends. The trend for the Jersey ASR rate for suicide can be seen in the graph below from 2017 Statistics Jersey Mortality Report.
Age-standardised mortality rate by intentional self harm per 100,000 residents (3 year average)
25
20
17.8
15 14.8
10 9.4 9.2 9.2 8.7 10.7
5
0 ![]()
2008-2010 2009-2011 2010-2012 2011-2013 2012-2014 2013-2015 2014-2016
For the 2014-2016 period, the rate for our nearest comparison in the South West of England was 11.2. The lowest recorded rate was London at 7.8 and the highest Northern Ireland at 18.1.
The 2017 Mortality Report showed the annual number of deaths in 2016 as 15 which can be seen in the graph below. This is the highest number of deaths in recent years with the next highest annual number of deaths being 12 in 2012. Fluctuations year to year are evident with the highest number recorded in 2009.
Deaths by suicide in Jersey
 26
26
15 16 15
12
![]() 10 8 9 8 10
10 8 9 8 10
2007 2008 2009 2010 2011 2012 2013 2014 2015 2016
Data on deaths by suicide is typically around 2 years in arrears to allow for accurate recording of deaths following conclusion of all inquests for the period. Therefore, deaths data for the previous two years cannot be confirmed. However, in reviewing inquests and reported sudden deaths indications suggest that in 2017 there will have been fewer annual deaths by suicide with less than 10, with 2018 returning to more than 10, although it is likely to be lower than in 2016.
Statistical methods aside, each individual death is a tragic loss to families and to our wider community. Unravelling the complexity of what lies behind suicide statistics is extremely difficult. Despite our Island's low numbers, any suicide is a tragic event, which often occurs as a consequence of complex combined multiple factors rather than one single isolated issue. Suicide is a challenging and sensitive issue in any community, and all the more so in a small one.
