The official version of this document can be found via the DOCX button.
The below content has been automatically generated from the original DOCX and some formatting may have been lost, therefore it should not be relied upon to extract citations or propose amendments.
19-21 Broad Street | St Helier
Jersey | JE2 4WE
Deputy Louise Doublet
Chair, Health and Social Security Scrutiny Panel
BY EMAIL
05 November 2024
Dear Chair,
Further to your letter of the 21st October 2024, please find below responses to your questions. Due to the unprecedented volume of detailed information requested for the 57 questions, I regret to inform you that we have been unable to provide a timely response to questions 8, 37, 38 and the section entitled Learning Difficulties – Specialist Accommodation'. Responses are being prepared as a matter of urgency and will follow shortly, under separate cover.
Contents
I-HCS-GP25-002 – In Vitro Fertilisation Funding
HCS-GP25-001 – Ongoing Risks and Pressures in HCS2
Replacement Assets and Minor Capital (HCS)
Digital Care Strategy – Extension
Learning Difficulties - Specialist Accommodation
Previous Government Plan 2024-2027
General
- Please can you provide details of any anticipated changes in service levels or access to care as a result of the proposed new budget?
Additional funding is provided to address a structural deficit in funding. This will increase HCS budgets from £286 million to £322 million in 2025, with the 2025 pay awards on top of this. Whilst the current service provision is expected to result in an overspend in 2024, closing the funding deficit in 2025 should enable current service provision to be maintained.
In addition, operational work already started should result in improvements to service access. For example, acute inpatient emergency care (General Medicine) is being prioritised alongside the permanent establishment of frailty Consultants. This will improve access to emergency care, ED performance and availability of beds which is expected to have a positive impact on Islanders waiting for elective care.
- Are you anticipating any further departmental reviews, GIRFT reviews, or similar to the maternity, rheumatology, and radiology reports, which may entail the need for additional funding and resources for specific areas within health?
Regular service audits and peer reviews are part of good governance in health and care services and contribute to the continuous improvement of services. Best practice in healthcare is continuously evolving through research, new technologies and treatments and clinical knowledge and experience. Whilst standards can be captured in documents, practical reviews from clinical peers who can provide feedback based on their wide range of expertise, is an effective way of review and audit. HCS clinicians also benefit from the personal interaction and discussions with experts from the UK.
HCS is committed to continuous learning from peer and specialist reviews, and which will be requested in liaison with clinical care groups and the Medical Director. The Royal College of Physicians is anticipated to undertake a review of Neurology Services in 2025.
- Can you explain the increase in other operating expenses' over the years 2025 to 2028?
This is due to annual increase in the Maintaining Health & Community Care Standards' funding over the years 2025-2028. This formula-based increase is supporting the maintenance of health and care standards through providing a continuous mechanism for funding increased costs in health and care. This is crucial in supporting services to maintain standards that constantly evolve and ultimately contribute to Islanders receiving modern clinical services.
- It is noted that revenue earned through operations is projected to remain static at £28,973,000 throughout 2025-2028:
- Do these projections account for any future inflationary increases?
Main sources of income include
- Private Patient Income
- Long Term Care Benefit
- Catering & Laundry
- Charitable and Medical Education Income
There is no income inflationary assumption built into the template at this time. However, inflationary increases will be decided through individual service assessment and agreed in line with the Public Finance Manual.
- Are any strategies under consideration to increase revenue earned through operations?
The private patient income strategy is to grow income from £12.2m in 2023 to reach £25m by 2028. This is described in the Private Patient Strategy 2025-28 which is published on gov.je.
- What specific improvement and innovation projects are being funded, and what outcomes are expected from these investments?
The following list of projects for 2025 were outlined in my letter dated 24 September 2024 titled Re: Budget 2025:
Finance Recovery Programme will continue in 2025 and consists of 6 workstreams:
- Workforce - Medical Staffing, Nursing Staffing, AHP, Non-Clinical
- Clinical Productivity - Theatres, Patient Flow, Off Island Acute Services
- Non-Pay, Procurement, Centralised Purchasing and Commissioned Services
- Medicines Management
- Income Maximisation - Private Patients, Other IMG schemes
- Digital Health
Capital Projects:
- Development of specialist accommodation for Islanders with learnings difficulties.
- Health Services Improvement Programme. An extension to the existing well-established essential maintenance programme continuing to address the most urgent Health and Safety requirements, across the health estate. With particular focus on keeping the Hospital compliant and operational until new facilities are available.
- Digital Care Strategy. Continuation of existing project to ensure continuous update of digital systems.
- Digital Systems Improvements. Delivery of an electronic patient record system for Mental Health and Adult Social Care Services.
- General Hospital Wi-fi. Implementation of upgrades and extensions to the hospital Wi-fi.
- Given the net revenue expenditure trends, what steps are being taken to ensure the financial sustainability of Health and Community Services?
The FRP Programme is made-up of six key workstreams with plans in place to achieve £25m of savings over 4 years and to establish long-term benefits through improved processes . These are:
- Workforce Productivity (Pay)
- Non-pay and Procurement
- Medicines management
- Clinical productivity (Theatres efficiency, Beds utilisation/Length of stay, Outpatients efficiency)
- Income
- IT and Digital
However, a number of risks to future increases in expenditure are outside of the operational control and require a long-term solution to increasing health and care costs.
- Increasing aging population and an increase in multi co-morbidities (contributing to increasing costs such as social care services, off-island care and treatment)
- Advancements in health and care treatments (for example, for medicines/drugs, medical equipment)
- Health inflation is higher than underlying inflation
- Page 91 of the Proposed Budget 2025-2028 states that the ongoing review has provided key insights into current spending and potential areas for healthcare funding reform. Can you share more details on the most significant findings so far, and how these are shaping the options being developed for future funding of Jersey's healthcare system?
The findings and insights which will inform potential options are broadly outlined on Page 92,
The Government Plan 2023 – 2026 noted that the Minister for Health and Social Services would undertake a review to better understand how we are spending money today, and to inform options for the future funding of our health and care system. This work has started and has provided some key insights:
- whilst Jersey's overall spend on health and care services is broadly in line with the OECD average, we spend more on hospital services and less on prevention and primary care services.
- household out-of-pocket spend is higher in Jersey than many other OECD jurisdictions (this includes payments to see GPs, dentists, and some hospital services)
- our funding system is more complex than other OECD jurisdictions which tend to favour a predominant source of funding (for example, predominately tax or employer / employee contributions), unlike Jersey's mixed funding system of tax, employer / employee contributions, out-of-pocket expenses, and private health insurance. Whilst this mixed system for raising funds is not problematic, the ways we govern the funds raised can make it harder for us to maximise effective use.
We also know that Islanders broadly support a collective approach to health care costs, as opposed to an individual approach – the majority of people believe we should all contribute to the costs of services provided to Islanders, as opposed to only paying for the services we use as individuals.
These insights will help inform potential options for change which will focus on how we:
- determine the best mix of funding that is needed in future?
- ensure the way we govern and spend the money raised supports best use of that money?
- contract with providers to deliver better value, safe, effective services?
- make decisions about the services needed across the health and care system? These options will be brought to the Assembly in 2025.
These options will be brought to the Assembly in 2025.
HCS Financial Recovery Plan
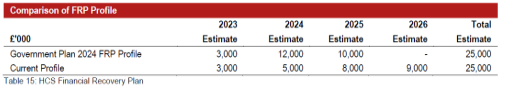
Figure 2 – Proposed Budget 2025-2028 (p48)
- What specific measures are being implemented to ensure that the £8 million in savings projected for 2025 and £9 million for 2026, will be achieved without compromising patient care?
The plans for 2025 and 2026 are based on a continuation of the Financial Recovery Plan (FRP) workstreams and supplemented by new opportunities as they are being identified by operational and clinical teams. The Financial Recovery Plan (FRP) is built on a set of core values that combine patient focused quality improvement, financial recovery, clinical, staff and stakeholder engagement, teamwork, and inclusive leadership to deliver sustainable improvements. Timely patient care and the quality of care are always considered as most important in any improvement activities – therefore, the FRP workstreams and projects have been developed and delivered on the core principle of quality and finance go hand-in-hand, and that better use of resources and efficiency is delivered by improving quality of care and the way we deliver it.
The FRP Report published in September 2023 provides further detail on the improvement projects.
- How will the FRP ensure long-term sustainability in delivering healthcare services while focusing on efficiency savings?
HCS will work operationally within their budget from 2025 (see also answer to question 1) and has measures in place through the FRP to deliver efficiencies and focus on on-going good budget management. However, the long-term sustainability of health and care provision is being separately addressed, please see answer to question 7 for more detail on potential options for change.
- Can you provide more details on how the revised timeline for the FRP was decided, and what factors influenced the decision to extend the savings timeline to 2026?
The main reason behind the extension of the savings delivery was the delay in having some of the enabling resources in place to deliver the savings whilst ensuring we maintain quality of care. For example, recruitment to substantive posts to remove agency/locum staff requires an active team of recruiters and HR processes to attract and on-board candidates which reduces time-to-hire. This took longer than originally anticipated due to longer setting up times and more challenging recruitment market conditions.
- Could you elaborate on the strategies being employed to optimise income generation as part of the FRP, and how these will contribute to the overall financial goals?
HCS income generation is primarily achieved through private patient services. The agreed 5-year strategy sets out the ambition and work plan and can be found on gov.je.
As I said in my foreword to the strategy, the private patient strategy signals a commitment to expand the choice of service provision to Islanders by enhancing the private healthcare offer, attracting skilled professionals to Jersey and increasing income to be used for the benefit of all Islanders.
Enabling choice is a key part of the way healthcare is delivered in Jersey and we must acknowledge that supporting this choice brings benefits to the whole system and is not detrimental to it. Our society is diverse, and encouraging private patients services can support a better balance of healthcare spending and prioritisation towards those who depend most on state funded care.
This strategy recognises and promotes the contribution made by private patients services to our whole Island economy. These services can support growth, not just for healthcare, and are a positive contribution to improving productivity in the workplace and diversifying the economy, continuing to make Jersey an attractive place to live.
Private patients services contributed £12.2 million to Health and Community Services (HCS) in 2023, which is approximately 5% of the overall HCS budget. Without patients using their private medical insurance or choosing to self-fund, Jersey's healthcare system and taxpayers would bear an additional financial burden.
- What measures are being taken to enhance procurement and contract management to ensure maximum efficiency and savings?
The FRP team and T&E's Commercial Services team continue to focus on priority procurement and contract management initiatives, which span the breadth of HCS. These initiatives are delivering efficiencies, whilst ensuring risks are managed appropriately by ensuring services are thoroughly understood and clinicians are involved when appropriate. Through regular engagement with Commercial Services, HCS staff are growing capability to undertake procurement and contract management activities. Governance, grip and control initiatives are being implemented to better understand contracted services and the associated spends, so that decisions which balance savings and clinical risk can be made effectively. Examples of the initiatives are:
- Reviewing all new supplier requests
- Improved governance with off-island acute care and review of spending profile
- Improving relationships with NHS Supply Chain
- Strengthened governance for tertiary care spend
We have also formed a Tertiary Care Steering Group to scrutinise and provide oversight over this sharply increasing off-island spend.
The tertiary services/off Island project team is focused on provision of improved grip and control of this growing area of HCS spend. The total cost of off-Island care is over £30m p.a. and rising at above inflation levels which provides significant opportunities to identify service and costs improvements.
HCS currently refers patients to over 40 NHS Trusts and during 2025 will work with consultants and Care Groups to review this range with a view to concentrating spend with fewer providers and consider much more strategic arrangements.
- What systems are being put in place to ensure effective staff management, resource allocation, and procurement improvements, as part of the FRP's cost-saving initiatives?
The FRP Programme is made-up of six key workstreams that target all these areas. Please see answers to question 12 above and question 15 below.
- How will the ongoing FRP be monitored to ensure that the savings targets for 2025 and 2026 are met? What contingencies are in place if these targets are not achieved?
The FRP is tracked, monitored and reported on a regular basis at:
- Bi-Monthly Finance and Performance Committee meetings
- Bi-Monthly HCS Advisory Board Meetings (in public)
New savings opportunities are identified as part of the FRP which is a rolling programme of continuous improvement. Where a shortfall in savings delivery is identified, recovery actions are taken, and mitigation schemes are developed to compensate as necessary.
- What specific measures were implemented in 2023 to achieve the £3.2 million in savings, and how will these strategies evolve to meet the £5 million, £8 million, and £9 million targets in subsequent years?
The FRP Programme is made-up of six key workstreams with plans in place to achieve £25m of savings over 4 years. These are:
- Workforce Productivity (Pay)
- Non-pay and Procurement
- Medicines management
- Clinical productivity (Theatres efficiency, Beds utilisation/Length of stay, Outpatients efficiency)
- Income
- IT and Digital
In line with the above workstreams, the savings delivered in 2023 are as follows.
FRP Savings Delivery FY23 | £'000 |
Nursing staffing (agency reduction and vacancy) | 187 |
Medical staffing (agency reduction and vacancy) | 279 |
AHPs staffing (agency reduction and vacancy) | 331 |
Non-pay cost reduction | 1,179 |
Drugs costs reduction (more efficient purchasing) | 98 |
Income generation | 1,145 |
Total | 3,219 |
Health Insurance Fund
- The Panel discussed the funding proposals for the HIF in its recent public hearing with the Minister for Social Security. As Minister for Health and Social Services, what is your view on how the immediate need for subsidies can be balanced with the long-term viability of the fund? How will GP subsidies be funded if the HIF runs out?
As MHSS, I fully recognise the importance of the primary care system and support the improvements in access to primary care services that have been led by the MSS.
Clearly there are a number of factors contributing to pressures in the HIF which include the additional subsidies recently agreed (for example, free GPs appointments for full time students), the pressures associated with health and care inflation (for example, rising drug costs) and demographic changes (the ageing population). But these are not problems for the HIF alone, we are experiencing these pressures throughout our whole health and care system.
We can contain some costs pressures across the system by:
- identifying and addressing areas of poor financial control (for example, HCS financial recovery work)
- investing in prevention schemes (for example, improvements to breast screening)
- supporting Islanders to live healthier (for example, public health awareness campaigns)
- establishing the structures and governance arrangements that support providers to work better together to tackle complex issues, such as keeping people safe and well at home (as per the current consultation on the Jersey Health and Care system).
Ultimately, however, we are going to have to invest more monies into health and care services, or accept a reduction in publicly funded services.
I intend to recommence the work on health funding reform, initiated by the previous MHSS, early next year with the proposed Health and Care Partnership Board providing advice and recommendations to myself and the Council of Ministers. It is clear that we need to develop long term sustainable solutions for Islanders as a whole.
In the meantime, I will continue to work closely with the MSS and any change to overall funding or HIF funding will take full account of the services funded by the HIF today.
- What strategies are in place to address the increasing healthcare costs associated with the Island's ageing population, particularly concerning the strain this places on the HIF.
See question 16 above.
- Minister, how do you plan to maintain or enhance access to primary care services for Islanders if the HIF's financial pressures continue to mount?
See question 16 above.
- To what extent could the planned expansions in healthcare services (e.g., free consultations, subsidised dressings) be at risk if the fund's depletion accelerates?
See question 16 above.
- Can you elaborate on how the implementation of the subsidised dressing scheme is working in practice? What feedback has there been from service users so far to date?
The scheme to provide free access to community prescribed dressings comes under the remit of the MSS and the costs are being met from the HIF. The MSS has confirmed that the first phase of the scheme is working well, involving FNHC and local community pharmacies. People with a medical need for dressings are referred on to the service, primarily by FNHC. The treating practitioner completes an order form which lists the dressings and products required by the patient. The patient obtains these from a participating pharmacy free of charge and the cost of the items is charged back to the HIF. Operational feedback from this phase is being gathered now to inform the permanent scheme. Customer feedback on the first phase of the scheme has been positive.
Both Community Pharmacies and FNHC have reported excellent feedback from patients. Pharmacies are reporting an increased demand for products since the scheme went live and have advised that patients are delighted they no longer have to pay for these dressings.
- What metrics or evaluations are in place to assess the effectiveness of the new contracts introduced in 2023 and 2024, such as the reduction in GP consultation fees and free services for children and students?
- How will you ensure that the additional subsidies provided to GPs are directly passed on to patients in the form of reduced fees?
The HIF contracts introduced in 2023 and 2024 fall under the responsibility of the MSS. The MSS has confirmed that all GP practices have entered into these contracts, which:
- reduce the adult copayment by a total of £30;
- provide free visits for children up to the age of 18; and
- more recently, provide free consultations for full time adults students
Practices are obligated to apply the agreed fee reductions under a contractual agreement. The fees charged by practices are monitored in CLS data systems to ensure compliance. This data shows the modal averages charged and enables the department to engage with the practice in the event that contractual terms were not applied. There have been no instances of non-compliance.
Up to date consultation fees are also published on gov.je
- If the HIF reaches a critical low before reforms are implemented, what contingency plans are in place to ensure Islanders' access to essential healthcare services is not disrupted?
See question 16 above.
I-HCS-GP25-002 – In Vitro Fertilisation Funding
- In the public hearing held on 19th September, the Panel was advised that a modelling system had been used to assess what budget would be sufficient based on known demand for IVF. Can you share the data and methodology used to model the funding allocation?
All the projections are estimates as sufficient data is not available to accurately determine demand or uptake.
Cost per cycle:
- The costs per IVF cycle varies depending on the clinic providing the IVF. For the purposes of the funding calculations an average figure of £6,169 was used as the cost of an IVF cycle including the necessary medications but not including the costs associated with frozen cycles.
- The costs associated with embryo freezing and transfer of frozen embryos varies. For the purpose of these calculations the average of freezing embryos is £818, with the average cost of a frozen cycle transfer being £2,723.
Calculating the number of cycles per year:
- As set out in the amendment to P20/2024, IVF is funded by the NHS in accordance with NICE guidelines in Scotland. In 2021 there were 2,924 NHS funded IVF cycles in Scotland. 2,924 equates to 58% of the total IVF cycles in Scotland that year, with a further 42% of IVF cycles being privately funded. Whilst a proportion of the cycles will be privately funded because the couple do not meet with NICE criteria, it is reported that a proportion of cycles are privately funded because of the waiting times associated with NHS funded IVF (target waiting time is 90% of patients have initial screening within 52 weeks) ie. the total number of IVF cycles that meet NICE criteria per year in Scotland is likely to be higher than 2,942 but, as more detailed data is not available, the figure of 2,924 is used for the basis of these calculations (equating to 87 cycles in Jersey).
- 2,942 cycles as proportion of population in Scotland equates to 87 cycles in Jersey meeting NICE criteria (albeit noting the numbers of meeting NICE criteria is likely to be higher).
- The proposed income thresholds were then applied to the 87 cycles to try to calculate the dampening' effect of the income criteria.
| First cycle | Second cycle | Third cycle | Total |
HEFA data re: % of couples who have 1, 2 or 3 IVF cycles per couple | 46% | 34% | 20% | 100% |
Estimated number of Jersey cycles (based on 87 cycles) | 40 | 29 | 18 | 87 |
Estimated proportion of cycles after dampening' effect of Jersey means test | No income test applied to first cycle so 100% of people who meet other criteria would get funded IVF | 91% of working age couples with no dependent children in Jersey have a income above £200k so would qualify for 2 cycles of IVF | 50% of working age couples with no dependent children have an income above £83,000 so would qualify for up to 3 cycles of IVF |
|
Estimated remaining cycles after dampening' effect of means test | 40 | 27 | 9 | 76 |
- Apply to proposed income criteria dampens demand from 87 cycles to 76 cycles that meet NICE criteria.
- 33% of IVF cycles will provide 2 addition viable embryos for freezing which based on 76 cycles equates to freezing costs for 25 IVF cycles.
- Of 25 cycles where embryos are frozen, 40% will have resulted in pregnancy from the initial fresh embryo transfer, leaving 60% (15 of the 25 frozen cycles) requiring frozen transfer at a later date. Statistically that equates to the 15 initial frozen transfer and 9 second frozen transfers ie. 24 frozen egg transfers in total.
Total cycles | 33% viable embryos for freezing | Frozen egg transfer 1 | Frozen egg transfer 2 | Total frozen egg transfers |
76 | 25 | 15 | 9 | 24 |
Total costs based on 76 cycles per year
Estimated costs | 2025 | 2026 | 2027 | 2028 | Total |
| £ | £ | £ | £ | £ |
IVF/ICSI cycle costs | £468,844 | £468,844 | £468,844 | £468,844 | £2,016,029 |
Frozen Embryo Cycle costs | £85,802 | £85,802 | £85,802 | £85,802 | £368,949 |
Counsellor staff pay costs | £73,153 | £73,153 | £73,153 | £73,153 | £292,613 |
Counsellor staff non-pay costs* | £2,200 | £0 | £0 | £0 | £2,200 |
Pharmacy Fridge | £4,000 | £0 | £0 | £0 | £4,000 |
IT Platform (OX-ar) Costs** | £11,700 | £11,700 | £11,700 | £11,700 | £49,080 |
TOTALS | £645,699 | £639,499 | £639,499 | £639,499 | £2,972,871 |
*NICE guidelines set out that counselling support should be provided to couples before they embark with IVF to supporting their decision making. during the process and after the process.
**Enhance IT platform required to support service improvements and monitoring
- It is recognised that, in addition to the income criteria, the funded IVF criteria as published are more restrictive in other areas that the criteria used in Scotland, for example:
- In Jersey the criteria provide that neither partner can have children from a previous relationship, in Scotland one of the partners may have children from a previous relationship
- In Jersey, the maximum number of IVF cycles includes any that the couple may already have had, even where the couple self-funded that IVF. In Scotland, the maximum number only includes previous cycles that were NHS funded.
- These additional restrictions are likely to result in less than 76 funded cycles per year but:
- there is insufficient data on which to calculate the impact of these additional restrictions on demand / reduced demand
- as set out above the 76 cycle figure was based on Scott ish data which it is known does not include all couple who are likely to be eligible for IVF
- whilst calculations were based on 76 cycles, the £620k funding provided for in the Government plan is only sufficient for 73 cycles
- no allowance has been made for a potential initial surge in 2025 and 2026 as couples previously excluded from funded IVF become eligible for the first time in Jersey.
NOTE:
The Minister for Health and Social Services is taking an appropriately cautious approach to IVF funding given the significant difficulties associated with understanding the impact of the proposed criteria, but a detailed monitoring system will be in place by 1 January 2025.
In the event that demand is below the anticipated 73 to 76 annual cycles, or the per unit cost of IVF can be reduced (there are ongoing negotiations with UK providers about the potential to secure a reduced cost in light of the overall increase in public monies being invested in IVF) the Minister will review and amend the criteria at end of Q1 2025.
- How was the figure of £620,000 determined, and what assumptions were made in this process?
See above.
- Did you adopt the National Institute of Care and Excellence (NICE) guidance for IVF funding and if not, why not?
NICE guidance is non-binding advice intended to assist the NHS to exercise its duty to deliver services. NHS Trusts are not compelled to deliver services against the guidelines, and in England and Wales most NHS Trusts' IVF provision does not accord with the guidance on the grounds of affordability.
P.20/2024, as lodged, proposed a new funding model for IVF which accorded with NICE guidance. The proposition was amended by a majority decision of the Assembly, removing the central proposition that IVF should be funded in accordance with NICE, and instead requiring the development of access criteria that accords with good clinical standards.
MHSS did not adopt the NICE guidance on the basis that:
- it is non-binding guidance
- funding in accordance with NICE guidance would create a significant additional investment requirement
- the Assembly did not direct that IVF services should be funded in accordance with NICE guidance.
- Given current infertility trends and the increasing average age of first-time IVF patients, how many Islanders do you realistically expect to benefit from this funding each year? Do you have data from your IVF travel bursary scheme which could help inform this calculation?
As set out above, based on the available public data is it estimated there up to 76 funded cycles of IVF may be provided per year. Increased infertility would result in more people receiving funded IVF as the service is not capped to a total of 76 couples.
The average age of first time mother in Jersey is 33 which is within the age criteria of 26 to 39 (or 40 to 42 which tests showing ovaries are likely to respond to treatment).
HCS does not have an IVF travel bursary scheme.
- What steps will be taken to ensure that the funding criteria are fair and inclusive? How will you address concerns that some individuals may be excluded from receiving funding?
It is recognised that criteria exclude some groups of people for example:
- single people of all genders
- same-sex male couples
- couples where one or both partners are already a parent
- couples who have already privately funded their own IVF treatment
- couples with higher household incomes.
As set out in the response to Question 31 below that are a numerous changes to the criteria that could be made to provide more equity of access and, in the event that of reduced costs and / or lower than anticipated uptake the criteria will be reviewed with a view to providing more greater equity of access.
- What steps will be taken to prevent financial incentives from driving patients towards IVF over other potentially suitable treatments
Couples will only be provided funded IVF where it is a clinically appropriate treatment for them. As set out in the criteria You must have exhausted all other preliminary treatments that have been clinically recommended before you can access funded IVF.
- What measures will be taken to ensure that couples opting for other infertility treatments, such as Intrauterine Insemination (IUI), are adequately supported and not financially disadvantaged?
HCS's assisted reproduction unit does not charge for the IUI procedure but the pathology lab does charge for preparation of the sperm (£350) where the sperm is donor sperm. Donor sperm is not required by many couples. IUI is provided on-island by the assisted reproduction unit, so there are no associated travel or accommodation costs for the couple.
- How will the effectiveness of the funding be monitored? Will there be a review process to assess the impact on those seeking IVF treatment?
The primary purpose of the funding is to support couples who are experiencing fertility difficulties to become parents. Pregnancy and live birth rates will be monitored to assess outcomes.
As set out above, a detailed monitoring system will be in place by 1 January 2025 to monitor update against the criteria. The criteria will be amended if they are found to be too restrictive.
- In our public quarterly hearing held on 19th September 2024 you advised that expanding the criteria to include same-sex female couples who currently face higher costs because they are required to have I.U.I. (intrauterine insemination) before they can access I.V.F, was something that you could not make an absolute commitment to but would be something you would be happy to discuss. When will you be in a position to make a firmer commitment on this and to share further details of what this would look like?
As set out above there are ongoing negotiations with UK providers about the potential to secure a reduced per unit cost for IVF in light of the overall increase in public monies being invested in IVF. In the event that costs are reduced (and / or the going monitoring of the access criteria indicate they are too restrictive), the Minister will review and amend the criteria at end of Q1 2025. Amendments to the criteria could include any of the following:
- removing restrictions on access by couples where one partner has children from a previous relationship
- not including previously IVF cycles in the maximum number of cycles where number of cycles, where those cycles were privately funded
- providing for IVF for single women
- further lowering the income thresholds
- removing the requirement for same-sex female couples (and opposite sex couples who do not have sex) to self-fund IUI before proceeding to funded IVF
- What consultation is taking place, if any, with the LGBTQ+ community on this matter?
There has been no consultation with regard to the proposed new criteria.
HCS-GP25-001 – Ongoing Risks and Pressures in HCS2
- Please can you provide a detailed breakdown of identified risks and pressures and further details of the prioritisation process and how the proposed £29.9 million will be spent?
The additional funding has been allocated to fund the underlying structural deficit funding. Pressures occurred in a range of services linked to increasing costs such as off-island placements, tertiary care contracts, increase in high-cost specialist treatments including high-cost drugs, and increasing demand for in-patient hospital medical care. See also answer to question 1.
- How was the figure of £29.9 million determined?
The breakdown of the growth funding is as follows:
Breakdown of Growth Funding | 2025 |
Activity Increases | 6.4 |
Tertiary Care contracts | 2.0 |
Estates and equipment (Building maintenance, service contracts, utilities) | 1.2 |
Non-Pay | 2.4 |
NHSE funding reduction | 0.5 |
Add back FRP Savings for 2025 | 8.0 |
FRP savings re-profiled into 2026 | 9.0 |
Exceptional Costs (including backpay) | 1.2 |
Less: reduction in Social Care costs for the Care at Home Cohort 2' group who are transitioning into the Long Term Care scheme | (0.8) |
Net Growth (before FRP Savings delivery) | 29.9 |
P-260024 – HCS Health Services Improvements (Backlog Maintenance)
- Please can a list be provided to the Panel of what the most urgent Health and Safety requirements across the health estate are and detail of the required timeframes needed?
Please see attached Appendix A
- Out of the known infrastructure failings, what work has been done to rectify major issues to date
Please see attached Appendix B
- What is the cause for the number of delays over the last 6 years with addressing red risk' items, which in turn, have now resulted in the amber risks' turning red?
Maintenance programmes and funding streams were aligned to the completion dates for delivery of the previous new hospital schemes (Future Hospital; Our Hospital). As these were not completed, the existing facilities continue to age and require intensive maintenance work. Whilst the work has been continuously risk assessed and prioritised it has also resulted in some risks that have previously been rated as amber' now being rated as red due to further deterioration of the facilities.
A limitation to addressing red risks are not only resources but also the availability of decant facilities. For example, to undertake work on wards in the hospital, beds and clinical areas need to be decanted to a different space.
- The Panel notes that £5 million is included in the Proposed Budget however it is your view that continued funding would need to be found on an annual basis from 2026 onwards until the new Health Facility is in operation. How much funding annually do you envision will be required and where do you foresee the budget coming from?
The Council of Ministers are aware of the on-going requirements for the existing hospital estate and infrastructure until the New Hospital Facilities Programme has been delivered. The HCS Estate team will continue to undertake their risk-based assessment aligned to the progress of the New Hospital Facilities Programme on an annual basis and identify required resources for inclusion in the proposed Budget 2026.
Digital Systems Improvement
- The Panel understands that the objectives and benefits were contingent on the commencement date of 1st October 2024 however the constraints of the allocated funding did not align with the recommended route of delivery. Did the ECR System project commence on 1st October 2024 and therefore receive the funding decision to implement Option 3? If not, what are the next steps?
The Electronic Care Record (ECR) System project has started with initial discovery stages which have informed the business case. The project has received approval to enter discussions with Commercial to progress with the procurement process. The team is currently working with Commercial to secure approval for issuing a request for quote (RFQ) to the supplier, followed by demonstrations. Subject to States Assembly approval of the 2025-2028 Budget the project will move into contract negotiations with the supplier based on option 3. There has been no significant change in the project's timeline at this stage and the team is working within the proposed allocation of the funding.
- What discussions have taken place to date to explore funding options from other departments such as CYPES?
The Electronic Care Record (ECR) System will have the functionality to be used across Adults and Children. Initial discussions took place with CYPES to explore shared funding options for the on-going revenue costs for licences and maintenance of the system. Further discussions are anticipated across departments to allow for continuity in exploring collaborative funding opportunities.
- How do you intend to mitigate the potential risk that Procured systems may not meet the specified requirement standards leading to service failures, additional costs and resources for development or replacement'?
To mitigate these risks the following strategies have been or will be employed:
- Comprehensive Requirements Gathering: A thorough requirements analysis has been conducted, involving all key stakeholders, including end-users, service users, carers, and subject matter experts, to clearly define and document system specifications. This engagement ensures that both current and future service needs are met, with a focus on future-proofing the system to adapt to evolving care demands.
- Rigorous Supplier Evaluation: A robust supplier evaluation process was carried out, allowing suppliers to demonstrate their capabilities. A comprehensive report on these evaluations has been submitted to the Commercial Team. Moving forward, an RFQ and demonstration process with the preferred supplier, incorporating an enhanced list of requirements, will be initiated. The supplier's responses will be integrated into the contract and will include testing against both functional and non-functional requirements to ensure the system fully aligns with our needs.
- Contractual Safeguards: Clear contractual terms will be established, including performance and requirements guarantees, SLAs, and penalties for non-compliance (subject to commercial review). This ensures that the supplier is accountable for delivering the agreed standards and requirements.
- Lessons Learnt: Previous experiences and lessons learnt from similar projects have been reviewed and incorporated into the process to avoid repeating past mistakes and ensure continuous improvement in procurement and implementation practices.
- Change Control Process: A formal change control process will be implemented to manage any system adjustments or enhancements during and after implementation. This process will ensure that changes are carefully evaluated and approved to prevent service disruptions or unplanned costs.
- Ongoing Monitoring and Feedback: During and after implementation, continuous monitoring of the supplier's performance and the system's effectiveness will take place. Regular feedback loops, such as end-user workshops and steering group meetings, will be established to ensure the system remains fit for purpose. Any risks that emerge will be addressed promptly.
By employing these strategies, we aim to minimise the risk of service failures and manage costs effectively, ensuring the system meets the required standards and facilitates seamless service delivery.
General Hospital Wi-Fi
- Please can you provide further information on what this new project entails and why these works are required in 2025?
The existing Wi-Fi in the hospital is variable in terms of capacity and coverage, which currently is a barrier to using digital health systems at the bedside and mobile across wards. The new Hospital EPR System investment will deploy further functionalities, and these new ways of working are largely mobile, digital at the patient bedside. New devices such as fluid monitors, e-observations, rely on reliable Wi-Fi to provide a safe level of care. The project will also address weak core network points at the same time as addressing the access points (the Wi-Fi kit in rooms), end to end, which are otherwise at risk of becoming bottlenecks in the network. This project addresses these issues and requirements and enables the strategic objectives of enhanced patient care and health outcomes and operational efficiencies. Further detail can be found in the Business Case which has already been shared with the Panel.
Replacement Assets and Minor Capital (HCS)
- What is the reason for the change in the proposed allocation from £2,500,000 to £2,250,000 in 2025 for this programme of works?
£2.5m was the original 2025 proposed allocation, however £0.25m from 2025 to 2024 to purchase equipment for HCS was brought forward to 2024 to support the procurement of critical equipment in 2024. As a result, the 2024 budget changed from £2m to £2.25m whilst the 2025 allocation has been reduced by £0.25m from £2.5m to £2.25m.
- Please can you provide further information on how the proposed £2,250,000 will be spent?
Items for the annual replacement plan of medical assets are currently being identified with clinical and operational teams. Equipment requested is usually used in theatres, radiology, clinical investigations, and clinical specialties.
Digital Care Strategy – Extension
- The Panel understands that in order to continue the implementation of the Digital Care programme, funding is needed to implement a number of areas. What is the risk should one area not receive the required funding?
- How would the lack of funding impact work already underway?
Should funding be curtailed to deliver the Digital Care Programme, this will have a direct result on productivity of the workforce, patient outcomes, capacity, patient safety and financial recovery. By underfunding projects, the delivery of intangible and cashable benefits will be hampered. For example, dual running of paper and digital systems, and reducing and optimising manual processes with digitised ones. Improving flow through enhanced and actionable business analytics, reducing administrative burden through a single digital system as opposed to part manual and part digital. Benefits realisation will be reliant on the funding, and the faster the funding is provided the faster the benefits are realised.
- Should funding be approved, what other Government initiatives do you foresee being reduced in scope or phased due to the completion of this project?
The funding and resource requirements have been planned and agreed with colleagues from Digital Services based on prioritisation of needs and impact. Prioritisation across the Government for digital projects is being undertaken regularly to ensure resources are being focused on projects with the highest impact and benefit.
Learning Difficulties - Specialist Accommodation
- Please can you provide a progress update on this project as well as the spend to date?
A response to Question 45 will follow as soon as possible.
- What are the key milestones for this ongoing project?
A response to Question 46 will follow as soon as possible.
- How do the projected amounts for £3,200,000 for 2026 and £1,624,000 for 2027 correlate to the project's original agreed allocation of £4,037,000 for 2024? Do they make up part of this amount or are they additional?
A response to Question 47 will follow as soon as possible.
- What is the reason for the proposed reduction in the project total from £9,350,000 to £8,850,000?
A response to Question 48 will follow as soon as possible.
- What is the rationale for no funding being required in 2025? Has the project been delayed? If so, why?
A response to Question 49 will follow as soon as possible.
Crematorium Resilience
- As Lead Minister for the Crematorium project, please can you provide further details on how you intend to modernise the crematorium'?
It is my intention to respectfully update the Crematorium in partnership with our key stakeholders. This will include updating the facility and also reviewing the furniture and equipment.
- Please can you detail what energy sources are being considered to power the hybrid cremator and how the options appraisal for this is being undertaken?
At this stage of the project initial scoping work is underway to consider all potential options for the hybrid cremator and once the preferred option has been agreed I will have further details about cost and timeframes which I am happy to share with the Panel.
- Can you provide the cost implications and timeframes for each option being considered?
See below.
- What are the timeframes and cost implications for ensuring all staff are fully trained to operate the new plant?
This will be dependent on the plant that is installed and commissioned. However, full training will be provided for all relevant staff.
Previous Government Plan 2024-2027
- The previous Health and Social Security Panel presented a comments paper to the previous Government Plan 2024-2025 highlighting its concern for the level of funding that had been determined for a new vaccination scheme, aiming to create an adult vaccination programme. Can you provide any information to the Panel regarding the extraction of money from the Health Insurance Fund to deliver the scheme in this year's Budget?
Adult vaccinations are delivered by either Primary Care, Public Health, sexual health teams, through Occupational Health services (such as HCS and Government of Jersey Immunisation team) and privately. The vaccines, and payment for delivering the services, are funded through a combination of the HIF, HIF Medical Benefit, contracts which access HIF funding, Public Health budgets, Occupational Health budgets and patient payments.
There is no extraction of funding from HIF to Public Health – the Minister for Social Security enters into agreements with community pharmacy and general practice for the delivery of some vaccinations (currently Covid and Flu), purchases vaccine for use in primary care settings (currently Flu, RSV and Shingles) and subsidises vaccinations undertaken in General Practice via Statutory Medical Benefit and Contracted Medical Benefit.
A number of vaccines are delivered by the Public Health team, including urgent responses to major disease outbreaks or other infectious disease threats e.g. MPox, measles. These are funded by Public Health.
In addition to delivering some vaccinations, the Public Health Vaccinations Team fulfils other functions, including:
- Providing specialist immunisation knowledge to primary care providers and the public
- Assessing children eligible for BCG vaccination and offering vaccination clinics
- Scheduling of baby immunisations (necessary to maintain high uptake)
- Scheduling of baby six-week baby checks
- Inputting data from the GP records into the child health system ensuring there is a comprehensive vaccination history
- Developing Patient Group Directives (PGDs)
- Conducting annual cold chain audits of GP practices and an annual stock check of vaccines in Primary Care
- Leading communications for vaccination campaigns e.g. COVID, flu, shingles, RSV.
Through the 2024–27 Government Plan process, £400k was allocated to Public Health, to continue funding the adult vaccination programme. This was intended to fund:
- 1 Health Protection Nurse
- 1 Vaccination Manager
- 1 Operational Lead
- 1 Analyst
- A small amount of non-pay cost
Funding was reduced by the 20% Government Plan growth reduction, resulting in a cost pressure. The shortfall has been met by reshaping other Public Health funding.
A vaccinations plan has been developed, the principles of which have been shared with the Minister for Health & Social Services. It includes the aim of streamlining and simplifying funding arrangements and ensuring resilience in delivery.
- Last year, the previous Panel expressed concern regarding the lack of detail about the increase in staffing levels over the last three years within Public Health. Can you provide further information into the rationale for this?
The picture of public health staffing in 2023 was complex because:
- the directorate was relatively new, had a range of new responsibilities and built from teams spread across the organisation. Baseline staffing numbers were difficult to calculate and staff transfers were not fully understood or taken into account,
- staffing numbers included those who were not part of the public health team, e.g. those delivering Major Incident health and wellbeing services (employed by HCS, but with the budget overseen by Public Health),
- the numbers included staff involved in offering a centralised adult vaccination service, which has since transferred to primary care,
- there were a range of budgets financing public health which added complexity and this complexity was difficult to communicate and understand.
The aim of the business case to maintain public health activities in 2023 was to secure recurrent funding for essential services, whilst offering a substantial budget reduction, bring together a plethora of budgets, reducing complexity and offer greater transparency about public health spending.
As part of the Government Plan debate, Public Health were required to secure approval from the States Employment Board prior to recruiting to the posts in the 2024 business case. This approval was achieved in February 2024 and the new structure implemented from 01 April. 18 posts were disestablished and 11 substantive posts established. A number of individuals were placed at risk of redundancy; some secured new roles and some left the organisation.
The Public Health establishment is robustly managed. Any vacancies are considered for re-structure to further improve capacity, skill-mix and value for money. Contracts for a number of fixed term, agency and contractor staff have not been renewed during 2024, and workloads have been reprioritised and/or reallocated to substantive staff.
- The previous Panel recommended that "Ahead of the debate of the Government Plan 2024-2027, the Minister for Health and Social Services must provide details of how many existing public health staff the requested monies under the revenue expenditure growth "maintaining the public health and health protection funding" will fund". It was noted that the figures of the estimated staffing levels for this year (2024) may be subject to change due to information based on assumptions. Please could you provide the Panel with an up-to-date FTE figure of the staffing levels for this year and for 2025, and whether there is any underlying growth for next year?
Currently the Public Health establishment is 51.3 FTE (the includes filled and current vacancies). 37.1 FTE staff are currently in posts, and an additional 10.6 FTE are held by temporary staff (i.e. in fixed term posts, employed as specialist advisors or cover for maternity leave). As at October 2024, a further 4 posts for the Major Incidents health and wellbeing support are employed in HCS or CLS.
The public health budget will reduce in 2025-6. The budget will reduce by approximately 14% in 2025 compared to the 2023 baseline. In 2025, a further two vacant posts will be disestablished, in addition to the 11 Public Health and 4 Major Incidents posts disestablished in 2024. A further budget reduction is planned in 2026 which will bring the total budget reduction to 18%.
- During the previous Government Plan, the previous Panel recommended that "the Minister for Health and Social Services must ensure that funding is identified in 2024 to improve and enhance the breast cancer screening service." What funding was identified, if any, and how has any additional funding improved the service?
An enhanced breast screening service will start by end of 2024. This will enhance the service and enable the roll out of a opt out' breast screening service. The opt out' service will ensure that all eligible women are automatically being contacted for a breast screen rather than relying on women contacting the service to opt in' for the screen. The additional equipment for this service has been funded through the John Clive Le Seelleur Fund, and additional staffing is funded through charitable funding for the next three years. The existing mammography unit is currently being replaced and is funded by the HCS departmental capital equipment budget.
Yours sincerely,
![]()
Deputy Tom Binet
Minister for Health and Social Services
D +44 (0)1534 440540
