The official version of this document can be found via the PDF button.
The below content has been automatically generated from the original PDF and some formatting may have been lost, therefore it should not be relied upon to extract citations or propose amendments.
Tom Leveridge
Scrutiny Office
States Greffe West End Donor Centre Morier House 26 Margaret Street St Helier London
Jersey JE1 1DD W1W 8NB
Sent via e-mail to: t.leveridge@gov.je
7th March 2018 Dear Mr Leveridge,
Jersey Organ Donation Review
I am writing in response to the letter from Deputy R J Renouf (Chairman of the Health and Social Security Scrutiny Panel) to my colleague Louise Davey, seeking information regarding organ donation and transplantation. This letter has been passed to me for a response, as I am currently leading work with NHSBT to support the various Government initiatives to introduce an opt out system for organ donation.
To respond to the queries in the order in which they are raised:
- Copies of questions that the next of kin of potential organ donors are asked Guidance on the discussion with the next of kin regarding the potential for organ donation, including the questions that should be asked, is available at the following sections of the Organ Donation and Transplantation website:
- http://www.odt.nhs.uk/deceased-donation/best-practice-guidance/consent- and-authorisation/
- https://nhsbtdbe.blob.core.windows.net/umbraco-assets- corp/1581/approaching-the-families-of-potential-organ-donors.pdf
Guidance on the questions to be asked once consent for donation is in place is provided in the enclosed document FRM4211'.
- What information is stored on the Organ Donor Register? The following data is stored on the Register:
- Title
- First Name*
- Other Name
- Last Name*
- Preferred Name
- Date of Birth*
- Sex* (male, female, other, prefer not to say, transgender)
- Ethincity
- Religion
- Address*
- Postcode*
- Telephone
- Mobile
- Donation decision: 'Opt-in', 'Opt-out' or 'Nominate a representative'
- Donation choices (which organs/tissue they would like to consent to donate):
Kidneys, Heart, Liver, Corneas, Lungs, Pancreas, Small Bowel, Tissue
- Withdrawal reason and date (for those that have previously registered and subsequently decided to withdraw from the register)
- Unique Identification Number(s)
NHS Number (English, Welsh, NI residents)
CHI Number ( Scott ish residents),
DVLA Number
DVANI Number (Northern Ireland residents)
Death Status
Date of death
(* Indicates Manatory Fields)
It should be noted that the data regarding ethnicity and religion are not made available to the operational teams at the point of determining the recorded decision of a potential organ donor.
- Who has overall responsibility for the Organ Donor Register?
The Chief Executive of NHS Blood and Transplant, Ian Trenholm, has overall responsibility for the Organ Donor Register.
The Head of the Organ Donor Register, Alex Hudson, also has Information Governance responsibility and is the Information Asset Owner for the Register within NHS Blood and Transplant.
- Where is the Register stored?
The Register is stored within the EU on the Microsoft Azure Cloud (Republic of Ireland and Netherlands). A copy of the register is also stored on an NHSBT server.
- How is the Register maintained?
There are a number of approaches for ensuring the Register is effectively maintained:
- The ICT support and maintenance of the Register is provided by a Third Party Supplier (Northgate Public Services).
- The general operational service, such as identifying and addressing any potential conflicts in data and responding to requests for the establishment of nominated representatives for organ donation, is provided by a team within the Organ Donation and Transplantation Directorate within NHS Blood and Transplant.
- The Register's website is maintained by the Digital Team within the Communications Directorate of NHS Blood and Transplant.
- Work to raise awareness of the Register and campaigns/ marketing activity falls within the responsibility of the Communications Directorate of NHS Blood and Transplant.
- Who has access to the Register?
The following people have access to the Organ Donor Register:
- Specialist Nurses for Organ Donation and Tissue Donation Nurses employed by NHS Blood and Transplant access the Register to determine if the potential donor had recorded a decision.
- Administrative teams within NHS Blood and Transplant. This includes the teams responsible for ensuring the Organ Donor Register data is accurate. It also includes the ODT Hub Operations team, who are responsible for liaising with the Specialist Nurses for Organ Donation.
- Staff working within the Organ Donor Line team, who respond to calls from the general public wanting to record a decision on the Organ Donor Register. This is provided by a third party contact centre – TelePerformance.
- On what basis can the Register be amended?
Data on the Register can be amended by members of the ODR and Organ Donor Line teams, in line with requests from the individuals concerned or, where appropriate, their representatives. For example, individuals can request an amendment – such as a change of surname or decision about which organs they want to donate – by inputting data to the Organ Donor Register website or calling the Organ Donor Line. The teams will amend data on the Register in line with their request.
- What happens if an individual changes their mind?
They are able to amend their registration decision (opt-in, opt-out) and/or their individual organ preferences via the website, by calling the 24/7 Organ Donor Line or make an amendment request in writing. Individuals have the right to access their own data and to be forgotten.
- Can a legal representative amend a donor's choice on their behalf?
Yes - there is a process to nominate an appointed representative to act on behalf of an individual regarding recording decisions on the Register. A parent can also amend the decision of a child under the age of 12.
- Are there any internal supervision and compliance procedures around the Register?
The Organ Donor Register complies with the requirements set out in the Human Tissue Act, the Data Protection Act and from May 2018, the General Data Protection Regulations.
NHS Blood and Transplant also has established reporting systems from the ODR to internal Clinical Governance, Quality and Information Governance standards. An internal performance report is made available to the Executive Team within NHS Blood and Transplant.
- Is there independent oversight of the Register?
The Register is subject to internal audits, which are currently overseen by Price Waterhouse Cooper (PWC)
- How does the process for triggering different teams from across the UK work in practice?
Clinicians in Intensive Care are responsible for referring potential donors to NHS Blood and Transplant. Once a referral is made, a Specialist Nurse for Organ Donation (SNOD) is mobilised to the hospital to determine the donation potential. If donation is a possibility, the SNOD will determine if any decision is recorded on the Organ Donor Register and approach the family to discuss donation. Once consent is given, the ODT Hub Operations team offers the organs for transplantation, in line with nationally agreed offering protocols (further data on this process is available at: http://www.odt.nhs.uk/transplantation/tools-policies- and-guidance/policies-and-guidance/.
Once organs have been accepted, the ODT Hub Operations team mobilise a Cardiothoracic and/ or Abdominal National Organ Retrieval Service (NORS) team to retrieve the organs. The NORS team also undertakes a range of checks during the retrieval process to assess the quality of the organs for transplantation. They will alert the relevant transplant unit if there are any concerns to agree whether the retrieval should proceed. In some cases, a Unit that had originally accepted the organ may then decline it. In these circumstances, the organ is re-offered through the ODT Hub Operations Team on a fast-track basis.
Once the organs have been agreed as suitable for transplantation, the ODT Hub Operations team organises the transportation of the organs to the relevant Transplant Units. The NORS team packs the organs ready for transportation and the ODT Hub Operations team alerts the Unit when they have been despatched.
- Are there any guidelines which apply to clinicians setting out how they should act in cases where organ donation is seen as a possibility? Could we provide a copy of these guidelines?
Best practice guidance on organ donation has been published by the General Medical Council, the UK Donation Ethics Committee and NICE. The ODT website contains details regarding best practice in identifying, referring and caring for potential organ donors. This is available at: http://www.odt.nhs.uk/deceased- donation/best-practice-guidance/donor-identification-and-referral/.
There is also best practice in consent. This is available at: http://www.odt.nhs.uk/deceased-donation/best-practice-guidance/consent-and- authorisation/
I hope that this has addressed your queries. Please do not hesitate to contact me if you require any further information (telephone: 07525299064; email: Claire.williment@nhsbt.nhs.uk). You may also find it helpful to look at the Organ Donation and Transplantation website (www.odt.nhs.uk), which contains a wealth of information regarding the organ donation, retrieval and transplant process.
Yours sincerely,

Claire Williment
Head of Opt Out Development
|
|
|
|
|
|
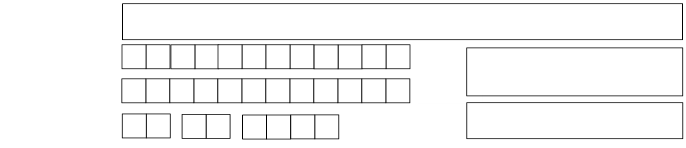
Patient Assessment Form
Directions for completion
1 This form must be completed in black or dark
blue ink by the Specialist Nurse – Organ Donation (SNOD)/Nurse Practitioner (NP)/Assistant Nurse Practitioner (ANP)/Tissue Transplant Co-ordinator and signed where required.
2 The original copy should be retained by the
SNOD/NP/ANP/Tissue Co-ordinator for the donor file.
3 A copy should be made for the patient's medical records. 4 In the event of organ and tissue donation, a legible
copy should be sent to the relevant Tissue Establishment, where required.
NOTE: The term patient is used throughout the form
to refer to the potential donor.
|
|
|
|
|
|
PATIENT INFORMATION | ||||||||
Hospital Number Cause of CHI Number Death NHS/CHI Number CHI Number Occupation Date of Birth (dd/mm/yyyy) | ||||||||
INTERVIEWEE INFORMATION | ||||||||
Information discussed with
| ||||||||
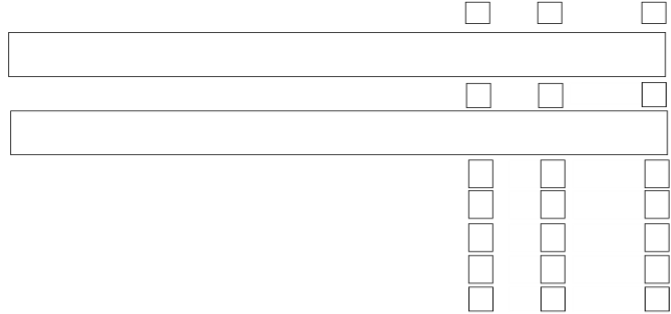
For patients under the age of 18 months or those who have been breast-fed in the last 12 months the mother is required to answer these questions with regard to both her own and her child's health. For children: has your child been breast-fed in the past 12 months? Yes No Unknown |
| |||||||
| No |
| Unknown |
|
| |||
GENERAL HEALTH INFORMATION | ||||||||
If YES, give details 3 a) Did your relative have diabetes? Yes No Unknown If YES, were they on insulin? Yes No Unknown 3 b) Is there a family history of diabetes? Yes No Unknown If YES, is it insulin-dependent diabetes? Yes No Unknown 4. Did your relative take regular medication? Yes No Unknown If YES, give details | ||||||||
|
|
|
|
|
|
GENERAL HEALTH INFORMATION |
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
5. Did your relative ever undergo any investigations for cancer or were they ever diagnosed with cancer? | Yes |
| No |
| Unknown |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If YES, give details |
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unknown |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, give details |
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
|
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unknown |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, give details |
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
| No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, give details |
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
|
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, give details |
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
|
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unknown |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Give details including date |
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
11. Did your relative ever have an organ or tissue transplant? | No Unknown | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, give details including date |
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, give details of where, when and the reason |
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
GENERAL HEALTH INFORMATION |
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
13. Did your relative receive a transfusion of blood or blood product(s) at any time? | Yes |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, give details including where, when and reason for transfusion |
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
14 Did your relative suffer from recent memory loss, confusion or unsteady gait? | Yes |
| No | Unknown |
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, any reasons for this? |
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unknown |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Alzheimer? |
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If YES, give details |
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
|
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
they ever told that they were at risk of prion disease? |
|
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If YES, give details |
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
17. Did your relative ever receive human pituitary extracts, e.g. growth hormones, | Yes |
| No Unknown | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
fertility treatment or test injections for hormone imbalance? |
|
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If YES, give details including dates |
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
18. Did your relative suffer from any chronic or autoimmune illness or disease of | Yes |
| No Unknown | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
unknown cause? |
|
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If YES, give details |
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
19. Did your relative ever have hepatitis, jaundice or liver disease? | Yes |
| No
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, give dates, diagnosis, treatment and location |
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
No |
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, give details, and any treatment received |
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
RECENT HISTORY |
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
21. Did your relative have any signs of recent infection, e.g. colds, flu, fever, night sweats, swollen glands, diarrhoea, vomiting or skin rash? | Yes |
| No |
| Unknown |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If YES, please specify dates, symptoms, diagnosis, and treatment |
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
| No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If YES, give details |
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
| No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
or cosmetic treatments that involve piercing the skin in the last 4 months? |
|
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If YES, give details including where and when |
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
| No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
with a bat anywhere in the world, or been bitten by any other animal whilst abroad? |
|
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If YES, give details of incident, circumstances, animal, place, dates, and treatment. |
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TRAVEL HISTORY |
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
25. In the last 12 months did your relative go outside the UK (including business | Yes |
| No |
| Unknown |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
trips)? |
|
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If YES, give details of dates and destinations visited |
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
the UK for a continuous period of 6 months or more? |
|
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, give details of dates visit/return and destinations |
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
have picked up whilst abroad? |
|
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If YES, give date of fever/illness, places visited, duration and dates |
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
continuous period of 4 weeks or more? |
|
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If YES, give details of dates, places (rural/urban areas), nature of visit |
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, give details of date and place |
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
BEHAVIOURAL RISK ASSESSMENT |
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
29. Did your relative (a) Consume alcohol? Yes |
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unknown |
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, what and how much? |
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No |
| Unknown |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, give details |
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No |
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(b) Has ever injected, or been injected, with non-prescription drugs, including Yes body-building drugs, even if it was a long time ago or only once? |
| No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(c) Been in prison or a juvenile detention centre for more than 3 Yes consecutive days in the last 12 months? NB This excludes those who have been in a police cell for <96 hours 31. Was your relative ever sexually active? Yes |
| No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unknown |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If no, go to question 33. If yes, is it possible that your relative: (a) Was ever given payment for sex with money or drugs? Yes |
|
|
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unknown |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(b) Ever had a sexually transmitted disease? Yes |
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unknown |
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If YES, give details |
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
If no, go to question 33. If yes, is it possible that in the last 12 months your relative |
|
|
|
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
had sex with: |
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(a) (for male patients only) another man? Yes |
| No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(b) (for female patients only) a man who has had sex with another man? Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(b) (for female patients only) a man who has had sex with another man? Yes |
| No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(c) Anyone who is HIV or HTLV positive? Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(c) Anyone who is HIV or HTLV positive? Yes |
| No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(d) Anyone who has Hepatitis B or C? Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(d) Anyone who has Hepatitis B or C? Yes |
| No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(e) Anyone who had a sexually transmitted disease? Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(e) Anyone who had a sexually transmitted disease? Yes |
| No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(f) Anyone who has ever been given payment for sex with money or drugs? Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(f) Anyone who has ever been given payment for sex with money or drugs? Yes |
| No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(g) Anyone who has ever injected drugs? Yes |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
(g) Anyone who has ever injected drugs? Yes |
| No |
| Unknown |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| (h) Anyone who may ever have had sex in any part of the world where Yes AIDS/HIV is very common (this includes most countries in Africa)? |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| (h) Anyone who may ever have had sex in any part of the world where Yes AIDS/HIV is very common (this includes most countries in Africa)? |
| No |
| Unknown |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33. Having answered all the previous questions, is there anyone else who you think Yes may provide more information? |
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
No |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If YES, please specify |
|
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
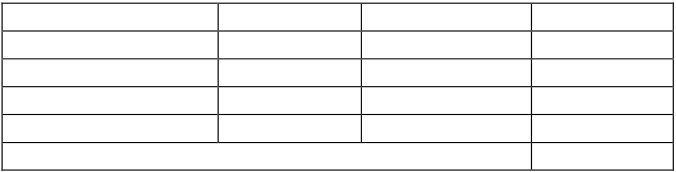
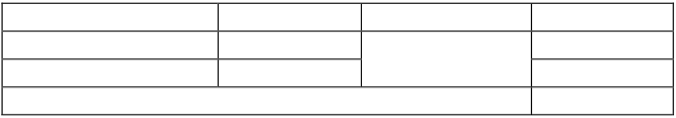
Question number | Relevant additional information. If any questions have been answered as unknown, give an explanation |
|
|
 Signature of healthcare professional obtaining information
Signature of healthcare professional obtaining information
Designation of healthcare professional obtaining information
2 | 0 |
|
|
Date of interview
FRM4211/3.1 Effective: 01/12/15
Please print name
 Time of interview
Time of interview
Page 7 of 9
|
|
|
|
|
|
CALCULATION FOR PLASMA DILUTION: | ||
Record ALL fluid administered in the 48 hours prior to taking sample for microbiology screening | ||
Fluid given. (Please give name, not just colloid or crystalloid) | Date and time administered | Vol. in millilitres |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
 Does a haemodilution calculation need to be carried out?
Does a haemodilution calculation need to be carried out?
| Reason |
|
Yes No
A haemodilution calculation must be performed if the patient has:
A - If the donor has received blood products/components, a pre-transfusion sample must be sought irrespective of volume of blood or blood product. This sample must be submitted for microbiological characterisation of the donor. B - If haemodilution calculation is 50%, a pre-dilution sample must be sought. If pre-transfusion or pre-dilution samples can not be found, the Microbiology laboratory and all recipient centres/ tissue establishments must be informed and this documented. * Decision on significance of blood loss should be discussed with clinical ITU team and made on a case by case basis. |
CALCULATION FOR PLASMA DILUTION continued |
INTERVAL PRIOR TO SAMPLING VOLUME INFUSED (ml) % RETAINED VOLUME RETAINED (ml) > 24 HOURS 0 None 2-24 HOURS 25 1-2 HOURS 50 <1 HOUR 75 TOTAL CRYSTALLOID RETAINED:
INTERVAL PRIOR TO SAMPLING VOLUME INFUSED (ml) % RETAINED VOLUME RETAINED (ml) 100 (Blood) 24-48 HOURS 50 (Colloid) 0-24 HOURS 100 TOTAL BLOOD/COLLOID RETAINED:
(CRYSTALLOID RETAINED+ BLOOD/COLLOID RETAINED) X 100 ESTIMATED TOTAL BLOOD VOLUME: BLOOD VOLUME 70ml per kilogram of body weight 50ml per kilogram of body weight in ICU ACCEPT (<49%)/REJECT (50%)
|