The official version of this document can be found via the PDF button.
The below content has been automatically generated from the original PDF and some formatting may have been lost, therefore it should not be relied upon to extract citations or propose amendments.
Organ Donation
Opt out? Neil MacLachlan
Family experience 2006
Ever thankful to the donor and their family 
 • Transfer from Jersey to London Easter 2006
• Transfer from Jersey to London Easter 2006
• Transplant June 16th 2006
• Back at school September 2006
• Durham University
• Love Hearts Appeal 2102


 Some interesting facts
Some interesting facts
• The first living organ donor in a successful transplant was Ronald Lee Herrick (1931–2010), who donated a kidney to his identical twin brother in 1954. The lead surgeon, Joseph Murray, won the Nobel Prize in Physiology or Medicine in 1990 for advances in organ transplantation.
• The youngest organ donor was a baby with anencephaly, 2015,who lived for 100 minutes and donated kidneys to adult in renal failure.
• The oldest known organ donor was 107 years Scott ish woman whose corneas were donated after death in 2016.The oldest known organ donor for internal organ was 92 year old Texan man whose family agreed to donate his liver after he die of stroke.
• The oldest altruistic living organ donor was an 85-year-old woman in Britain, who donated her kidney to a stranger in 2014 after hearing
how many people needed to receive a transplant.
A rare situation 
Although over half a million people die every year in the UK, fewer than 5,000 people will die in circumstances where they can become an organ donor.
You are more likely to be in a situation whereby you need an organ to survive than be in a situation where you can donate your organs on death.
Waiting is not easy 
 • Last year, 457 people died waiting for a transplant, including 14 children. There are currently 6,414 people on the transplant waiting list including 176 children. 3/day die waiting.
• Last year, 457 people died waiting for a transplant, including 14 children. There are currently 6,414 people on the transplant waiting list including 176 children. 3/day die waiting.
Jemima Layzel – 8 people saved
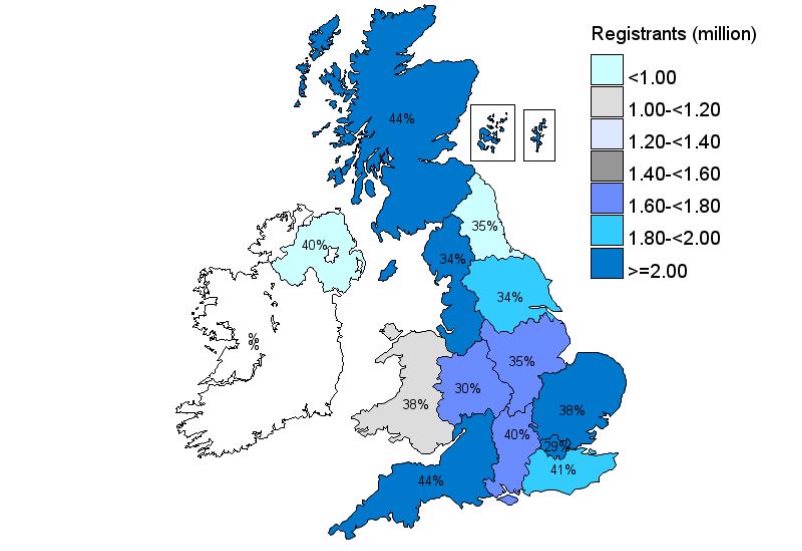
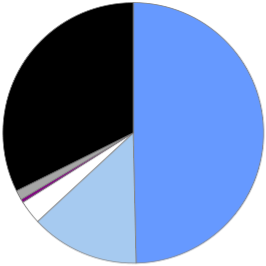
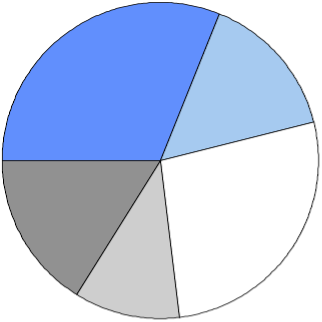
 Proportion of people who opted-in on the NHS Organ Donor Register by 31 March 2017, by Strategic Health Authority
Proportion of people who opted-in on the NHS Organ Donor Register by 31 March 2017, by Strategic Health Authority
 Neil MacLachlan
Neil MacLachlan
Source: Transplant activity in the UK, 2016-2017, NHS Blood and Transplant
March 2017
Jersey- 13,788 = 13.2%
July 2013, 9304, 9% Jersey
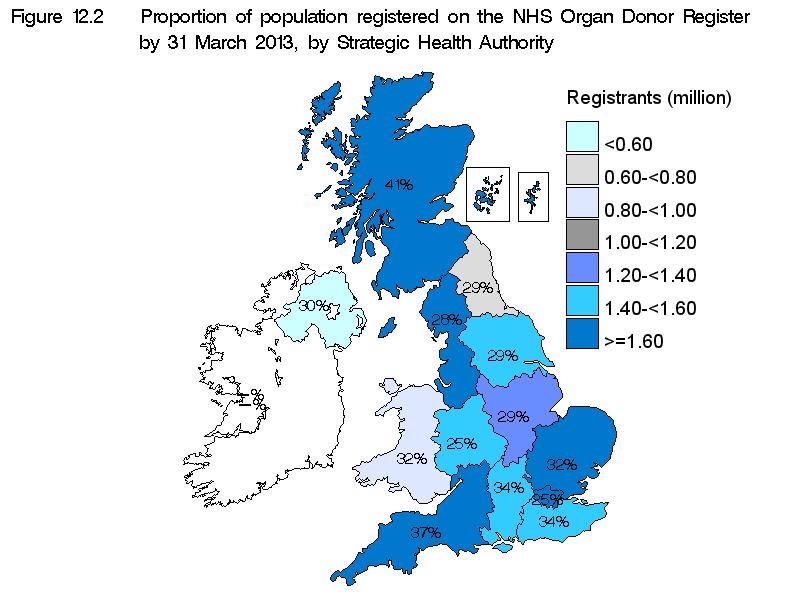
Source: Transplant Activity in the UK, N20eil 12Mac-20Lac13hlan(unpublished) and UK Transplant Regi
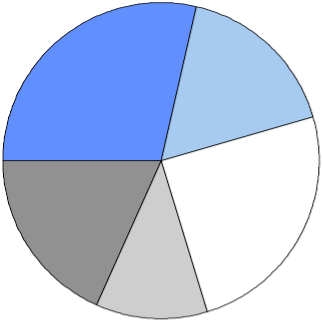
 Source of applications for opt-in registration¹ on the NHS Organ Donor Register, 1 April 2015 - 31 March 2017
Source of applications for opt-in registration¹ on the NHS Organ Donor Register, 1 April 2015 - 31 March 2017
2015-2016 2016-2017
 Online 32%
Online 32%
Paper 1%
Other
0% Boots
3%
GP registration 14%
Online 30%
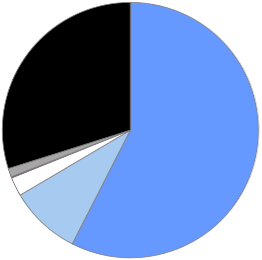 DVLA
DVLA
50%
Paper
1% DVLA 58%
Other
0%
Boots
2%
GP registration 9%
¹ Please note that a back-log of registration activity made via the UK GP Services is not accounted for in these figures. These registrations will be uploaded in due course and reflected in future reports
Source: Transplant activity in the UK, 2016-2017N, eil NHMSac BlooLacdhlan and Transplant
 www.organdonation.nhs.uk
www.organdonation.nhs.uk
• 95% people would accept an organ if necessary
• 13% on organ donation register in Jersey
• 36% on register in UK
• One register for all
• 3 people die every day waiting for organ
• 1000 die / year
• Every person has equal right of receiving organ
• 46% family refusal rate
Neil MacLachlan
 Age and gender of people registered on the NHS Organ Donor Register by 31 March 2012
Age and gender of people registered on the NHS Organ Donor Register by 31 March 2012
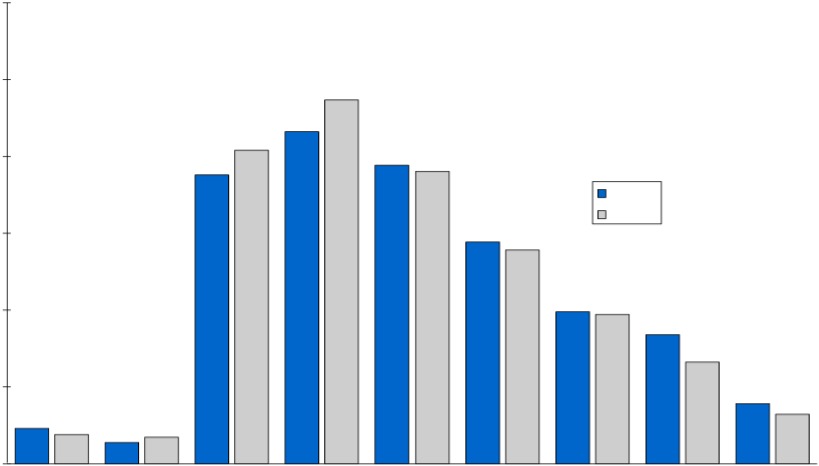 30%
30%
25% 23.7%
21.6%
20.4%
20% 18.8% 19.4%19.0%
Male
Female
15% 14.4%13.9%
9.9% 9.7%
10%
8.4%
6.6%
5% 3.9%
3.2% 2.3% 1.9% 1.4% 1.7%
0%
<11 11-15
16-20 21-30 31-40
Age group (years)
41-50 51-60 61-70 71+
 Registrants on the NHS Organ Donor Register, 1 April 2011 - 31 March 2012, and the general population, by socio-economic group
Registrants on the NHS Organ Donor Register, 1 April 2011 - 31 March 2012, and the general population, by socio-economic group
ODR registrants
 wealthy achiever 31%
wealthy achiever 31%
urban prosperity 15%
hard-pressed
16% comfortably off
27%
moderate means 11%
UK population
 wealthy achiever
wealthy achiever
urban prosperity 29%
17%
comfortably off hard-pressed 25%
18%
moderate means 11%
New strategy 
• NHSBT is working with stakeholders to develop a strategy to ensure that as many people as possible in the UK receive the transplant they need.
• We aim to increase the number of people having a transplant and this means increasing both the number and quality of donors/organs.
Organ Donation and Transplantation
Strategic Objectives to 2016/17
Portfolio of evidence
 Number of deceased donors and transplants in the UK, 1 April 2007 - 31 March 2017, and patients on the active transplant list at 31 March
Number of deceased donors and transplants in the UK, 1 April 2007 - 31 March 2017, and patients on the active transplant list at 31 March
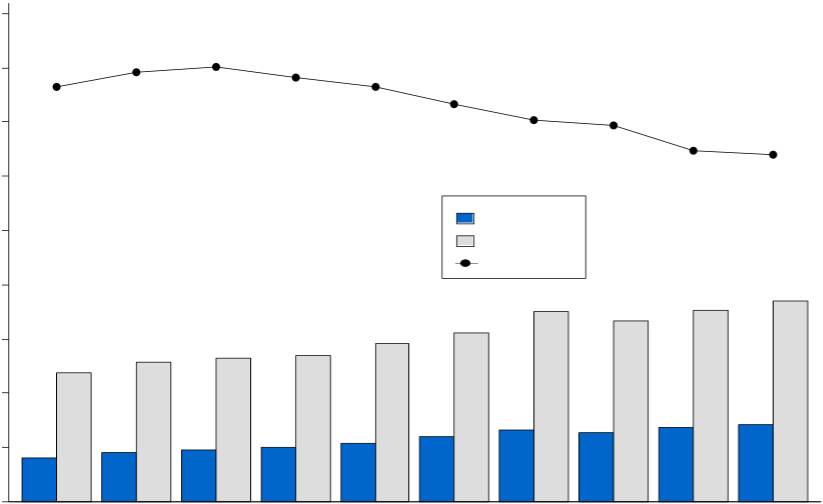 9000
9000
8000
7907 8012 7814
7661 7645
7000 7335
7026 6943
6469
6000 6388
Donors
5000 Transplants
Transplant list
4000 3710
3508 3528
3340
3118
3000 2569 2660 2706 2916
2384
2000
1212 1320 1282 1364 1413
959 1010 1088
1000 809 899
0
2007-2008 2008-2009 2009-2010 2010-2011 2011-2012 2012-2013 2013-2014 2014-2015 2015-2016 2016-2017 Year
 Number of deceased and living donors in the UK, 1 April 2007 - 31 March 2017
Number of deceased and living donors in the UK, 1 April 2007 - 31 March 2017
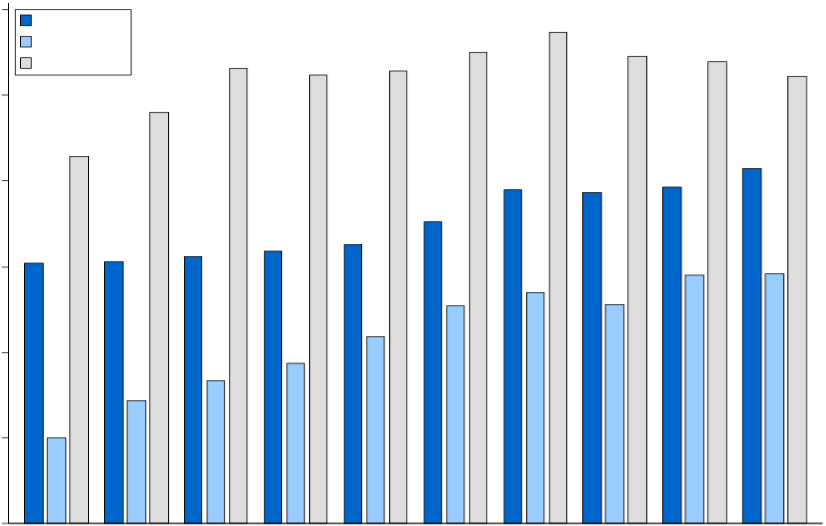 1200
1200
DBD donors 1148
DCD donors 1101 1092 1078
Living donors 1062 1046 1055 1043 1000 961
858
829
800 780 772 785
705
609 611 624 637 652
600 579 584
540
507 510
436
400 373
335
288
200
200
0
2007-2008 2008-2009 2009-2010 2010-2011 2011-2012 2012-2013 2013-2014 2014-2015 2015-2016 2016-2017 Year
 Age of deceased donors in the UK, 1 April 2007 - 31 March 2017
Age of deceased donors in the UK, 1 April 2007 - 31 March 2017
100 N= 3 5 8 10 11 12 11
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]() 809 899 959 1010 1088 1212 1320 1282 1364 1413 15 13 14
809 899 959 1010 1088 1212 1320 1282 1364 1413 15 13 14
90 17
15
18
80 20 23 22 22 22 23 22 70 24
26
24
60 23
25 26 22 25 25 24 50
40
50
30 48 46 42
20 38 37 37 39 36 36 10
0 5 7 4 4 4 4 4 4 4
2007-2008 2008-2009 2009-2010 2010-2011 2011-2012 2012-2013 2013-2014 2014-2015 2015-2016 2016-2017 Age
0-17 18-49 50-59 60-69 70+![]()
 Age and gender of total people registered as opt-in on the NHS Organ Donor Register by 31 March 2017
Age and gender of total people registered as opt-in on the NHS Organ Donor Register by 31 March 2017
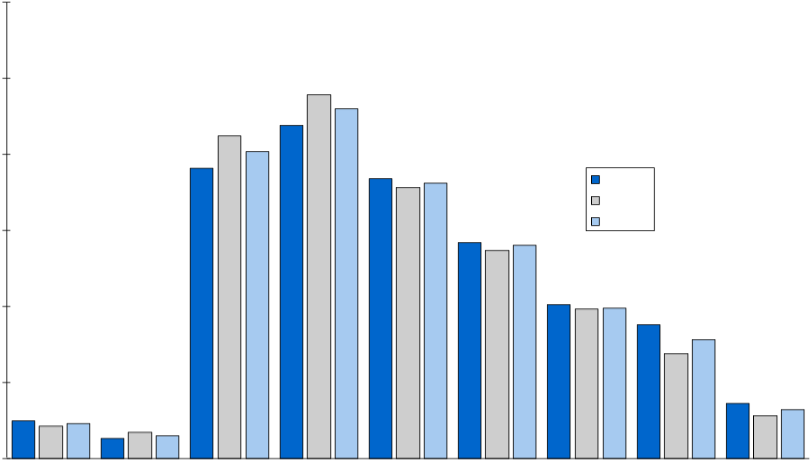 30%
30%
25% 23.9%
23.0%
21.9%
21.2%
20.2%
20% 19.1%
18.4% 18.1%
17.8% Male
Female
Total
15% 14.2% 14.0%
13.7%
10.1% 9.9%
10% 9.8% 8.8%
7.8%
6.9%
5%
3.6% 3.2% 2.5% 2.3% 2.8%
2.1% 1.7%
1.3% 1.5%
0%
<11 11-15 16-20 21-30 31-40 41-50 51-60 61-70 71+
Age group (years)
 Age of people registered as opt-in on the NHS Organ Donor Register between 1 April 2016 and 31 March 2017
Age of people registered as opt-in on the NHS Organ Donor Register between 1 April 2016 and 31 March 2017
 30%
30%
25% 24.4%
20%
18.0%
15.4% 15%
12.3%
10.9% 11.3%
10%
5.0% 5%
1.8%
0.9%
0%
<11 11-15 16-20 21-30 31-40 41-50 51-60 61-70 71+
Age group (years)
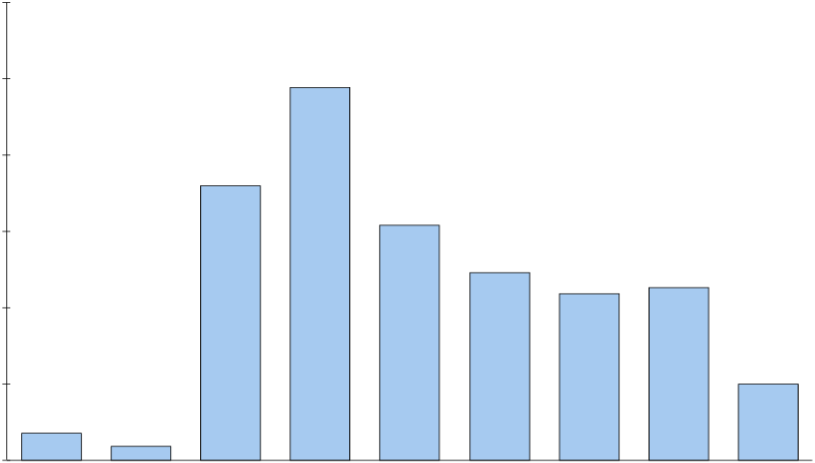
 UK potential deceased organ donor population, 1 April 2016 – 31 March 2017
UK potential deceased organ donor population, 1 April 2016 – 31 March 2017
 UK population1 ~65,000,000
UK population1 ~65,000,000
UK deaths2
~600,000
Deaths in hospitals3
~ 290,000
Potential donors4,5
7,024
Eligible donors4,6
5,681
Donation requests4
3,144
Consented donors7 2,082
Actual donors7 1,413
Transplants7,8 3,675
Organs transplanted7,8 4,025
1 Mid 2015 estimates: www.ons.gov.uk
2 2015 data: England & Wales www.ons.gov.uk; Scotland www.gro-scotland.gov.uk; Northern Ireland www.nisra.gov.uk
3 2015 data: England & Wales www.ons.gov.uk; Scotland www.isdscotland.org; Northern Ireland www.nisra.gov.uk
4 2016/2017 data: NHSBT, Potential Donor Audit
5 Potential donor - patients for whom death was confirmed following neurological tests or patients who had treatment withdrawn and death was anticipated within four hours
6 Eligible donor - Potential donor with no absolute medical contraindications to solid organ donation
7 2016/2017 deceased donor data: NHSBT, UK Transplant Registry
8 Using organs from actual donors in the UK
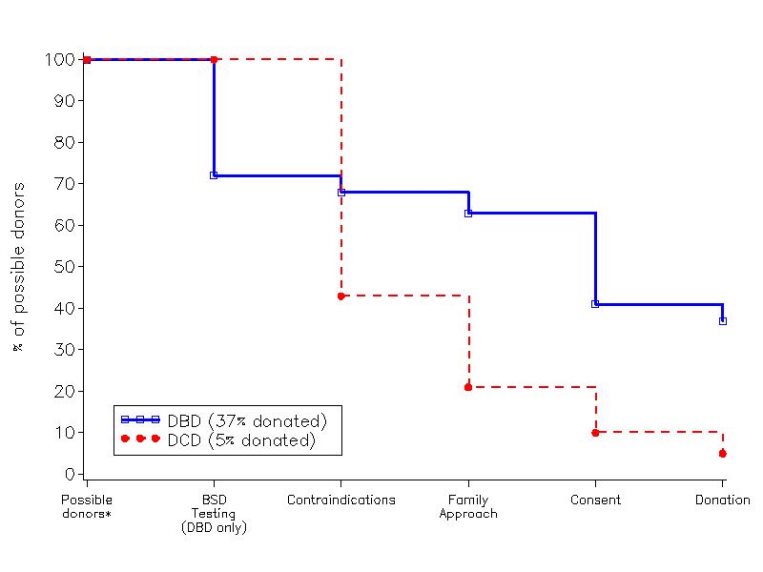
![]() DBD
DBD
28%
![]() 57% 4%
57% 4%
7%
35% 2010/11 10% 637 donors
53% (37% of possible)
49%
50%
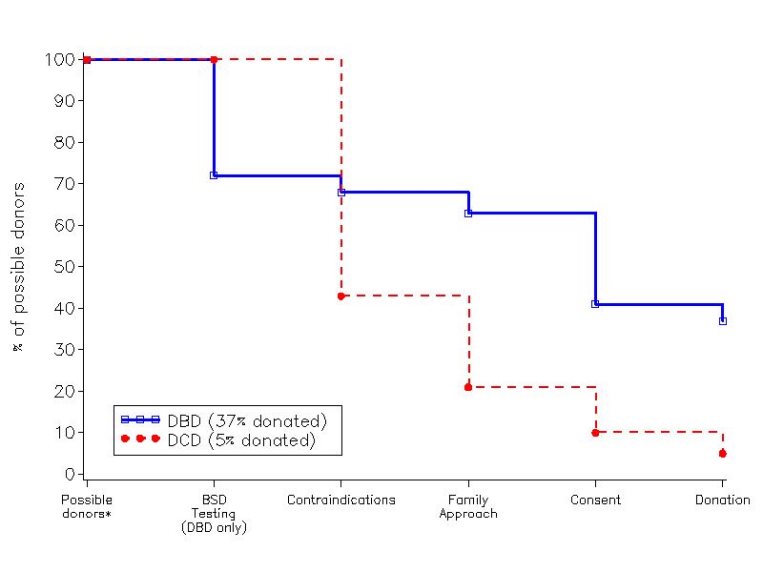 DBD DCD
DBD DCD
28%
57%
4%
7%
35% 2010/11 10% 637 donors
53% (37% of possible)
49%
50%
373 donors
(5% of possible, 12% of those not contraindicated)
Family refusal rates, 2010 
 45 43 40
45 43 40
35
31.5
29.9
30
25
20 19.3 19.2 19
15
10 8.7
7.1
5.8
4.7
5
0
UK Italy Romania Rep Ireland Croatia Spain Poland Slovakia Hungary Czech
Country Republic
Note – limited international data avaNileil abMleaconLac hlanfamily refusal rates
The deceased rights? 
• The Human Tissue Act 2004 does not provide families with a legal right to overrule the wishes expressed by the deceased person. However, the legislation allows discretion not to proceed with the donation if doing so would cause deep distress to family members.' This is why family attitudes towards donation remain crucial even if someone is on the Register (and why they will remain crucial in Wales even when people are deemed to have consented by default).
Knowing helps 
• Unless someone has registered with the Register or carries a donor card, their family and those close to them may not know their views on organ donation when they die'. When their loved one's wishes are unknown, and faced with a decision at a time when they are feeling vulnerable and distressed, 46% of families choose to donate their organs. The remaining 54%, with nothing-to-go- on' may feel that the safest course of action for them is to refuse permission for donation.
• In contrast, when families know their loved one wanted to donate - for example either via the NHS Organ Donor Register or via a previous discussion with their loved one about organ donation - their consent rate is 88%.
• This fact is the crux behind the proposed resolution.
The family input 
• It is possible for family members to make an organ donation decision on behalf of the deceased, or to overrule the deceased's decision:
People can become donors without having officially registered their wishes first if their family gives consent (last year 1,200 people became donors this way)
Family members can stop deceased people becoming donors even if they had registered their wishes to donate. 115 families did this last year.
 How do we make organ donation a normal part of Jersey / UK culture?
How do we make organ donation a normal part of Jersey / UK culture?
Donor behaviour change
IDEAS
• HSSD/NHS staff to lead the way
• Partnerships with big employers
• Big campaigns every year eg Love Hearts
• Local publicity stories
• Change consent system
• Make it part of your will
• Standard part of the education curriculum
• Targeted engagement programme with BME communities and the councils where they live
• More information about living and altruistic donation
 How do we make sure every eligible donor is given the opportunity to donate?
How do we make sure every eligible donor is given the opportunity to donate?
Perfect practice every time
IDEAS
• No refusal without a detailed conversation with a trained expert
• Allow all families to consider donation over a longer period
• Develop an ICU reimbursement tariff which reflects and rewards perfect practice
• A plan for efficient donor testing
• Dedicated bed in busy units
 What should we do to increase the pool of appropriate potential donors?
What should we do to increase the pool of appropriate potential donors?
Total hospital approach
IDEAS
• Donors from outside ICU & ED
• Uncontrolled DCD donors
• Increase ICU capacity when there is a eligible donor
• 48 hour watchful waiting' before treatment withdrawal
• Elective ventilation
• Cardiac Donation after DCD
DCD 
• INTERESTING CASE
• Female in their twenties with Idiopathic pulmonary fibrosis + awaiting lung transplant.
• She had contracted H1N1 and her respiratory failure progressed rapidly over the course of 4 days; she was admitted to ICU for non-invasive ventilation only (NIV).
• There was further deterioration over the next 2 days despite NIV and a decision was made with the patient that the priority was to keep her comfortable and to withdraw treatment.
• She was registered on the Organ Donor Register and despite intermittent confusion due to hypoxia, she directly expressed a wish to be a donor to the consultant during conversations about end of life care.
• Her family supported this decision and gave consent for solid organ donation.
• Donation after circulatory death occurred and both kidneys were successfully transplanted.
Total transplant rates 
Total transplant rates from deceased and living donors for
Europe and the USA, 2010
 100
100
90.1 88.9 88
90 83.5
80.4
80
73.1
68.4 68.2
70 63.7 63.2 62.2
59.3
60
52.3
49.1
50
41.3
40 37.9 35.4
28.7
30
20 14.9 10
0
USA
Croatia Norway Portugal
UK
Spain France Sweden GermanyDenmark
Switzerland
The Netherlands Neil MCacouLacntryhlan
Italy
Finland Slovakia Hungary
Poland Latvia Greece
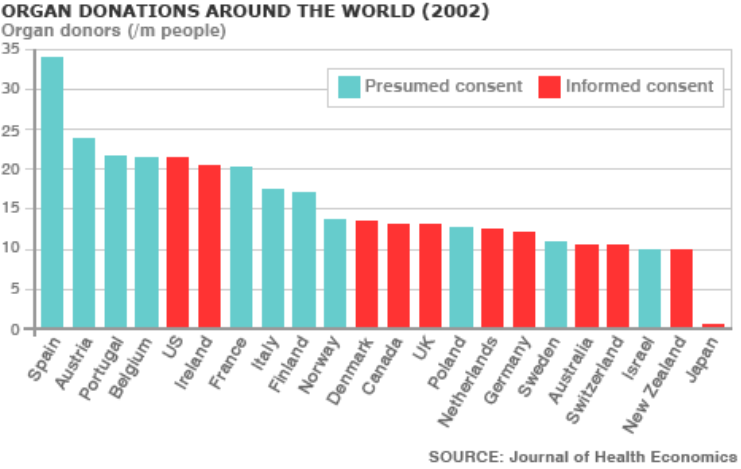
Consent by country 
Wales 2015 
 • spent more than £3.4m on a publicity campaign that has seen every household in Wales receiving a leaflet through their door, as well as TV adverts, supermarket roadshows and flashmobs at Cardiff train station.
• spent more than £3.4m on a publicity campaign that has seen every household in Wales receiving a leaflet through their door, as well as TV adverts, supermarket roadshows and flashmobs at Cardiff train station.
 Is Opt out necessarily best way?
Is Opt out necessarily best way?
• In the English system there are two groups of people: those who have opted in and registered their wish to be a donor, and those who have done nothing whose families will be asked to decide.
• In Wales there are now effectively three groups of people: those who have opted in and so registered their wish to be a donor; those who have done nothing for whom it is assumed they are happy to donate their organs, but it is still ultimately for their family to decide; and a third group who have opted out and so expressly registered their wish not to be a donor.
• As it currently stands, 6% of the Welsh population has opted out of organ donation. This is a group of people who in an opt-in system were still potential donors, depending on their families' wishes - they may not have ended up donating organs, but we just don't know.
Other factors important 
• There is correlation between countries having opt-out schemes and having a higher number of organ donors.
• But the countries which have the most donors per head combined the introduction of their opt-out schemes with other changes, like better infrastructure, more funding for transplant programmes and more staff working to identify and build relationships with potential donors before their death.
• Spain is often touted as an opt-out scheme success story.
• So-called "presumed consent" legislation was passed in 1979 but donor rates only began to go up 10 years later when a new National Transplant Organisation (ONT) was founded which co- ordinates the whole donation and transplantation process.
Hard Opt out? 
• In both Spain and Wales, families of potential organ donors are always given the chance to refuse. But this is not universal - Austria and Singapore both have "hard opt-out" systems where those who have not opted out are presumed to have consented to organ donation regardless of their families' wishes.
• And there are other differences, for example in Israel a priority incentive scheme means those who have agreed to donate their own or a deceased family member's organs are given priority on transplant lists should they themselves need an organ in the future.
• In "hard opt-out" systems there were increases in the organ donor rate of up to 25%.
Jersey – need to do more 
• Awareness – primary health care, schools, work place
• States of Jersey – driving license
• End of Life Care
• SN-OD local ( specialist nurses)
• DCD – introduce in line with UK
• Increase ICU capability
 Problems encountered
Problems encountered
• Primary Health Care – GPs want payment fro time spent discussing subject?
• Driving License – transfer data from Jersey to UK has been a problem
• High bed occupancy and theatre space limited in JGH.
• Public lack information
SUMMARY 
• Because there are problems with the 2 main routes of signing the OD register in Jersey, and because we have by far the lowest registration rates ( next to Guernsey) in the UK, then moving to an opt out system is sensible – but with this must come investment in other areas as happened in the Spanish ONT - eg.education, medical organisation.